"Merciless In Seattle: Untreated Pain, Misery, And Suicide" (November 2nd) examined the tragic suicide of Seattle resident Denny Peck, who had the misfortune of being dependent upon opioid drugs to manage his intractable pain that resulted from an accident that crushed part of his spine in 1990. When the pain clinic that had been treating Peck abruptly closed, he could not find a doctor who was willing to prescribe the drugs that made his life bearable. Two days following Peck's desperate, but futile call to 911, during which he maintained that he couldn't bear the pain anymore, Peck committed suicide by shooting himself in both side of his head. What happened to Peck is now considerably more likely to happen to you.
By any measure, it is now more difficult for patients with legitimate needs to obtain the powerful opioid pain-killers that they need just to function. Much of the blame for this changing paradigm has been placed at the feet of the CDC. You don't need to look very hard to find stories of both individuals and organizations who have expressed dismay at the agency's recent "voluntary guidelines" to physicians regarding opioid prescribing practice. David Hendry, writing for the Pain News Network called the CDC's advice to doctors as "the phrasing and logic of an extortionist."
There is no question that many people have been impacted by their inability to get the drugs that they had used responsibly for years. Both individuals and organizations have called the new rules Draconian.
But, has there been any benefit of these new guidelines to society as a whole? Or is this just another knee-jerk government reaction that will make the solution worse than the problem. It is too soon to have hard data on the impact of stringent opioid restrictions, but given historical precedent as well as fragments of emerging information, it is all but certain the effect of limiting opioids have had a downside. Perhaps even more than an upside.
The first "real life" example of the rapid decline of prescription opioids was seen in 2010—the year that OxyContin, the major driver of narcotic addiction, was reformulated to be abuse-resistant. It worked. But not as expected, which is shown in the graph below.

Once abuse-resistant OxyContin (pure oxycodone, the opioid medication in Percocet) was approved in 2010, its use immediately declined by 66 percent. But, between that time and 2013, overdose deaths from heroin (more accurately heroin and/or fentanyl) more than doubled, as addicts were forced to turn to these cheaper, more available, and more dangerous drugs. Not only did heroin/fentanyl overdose deaths go through the roof, but outbreaks of HIV (from needle sharing) were subsequently seen in Indiana, Kentucky, and Tennessee.
This same trend was seen in different forms in different areas of the country.
For example, a 2016 report entitled "Data Brief: An Assessment of Opioid Related Deaths in Massachusetts 2013-2014," showed a similar trend: that narcotic overdose deaths are skyrocketing, but it is not the pills that are responsible for the increased death. The real damage is being done by pill alternatives.
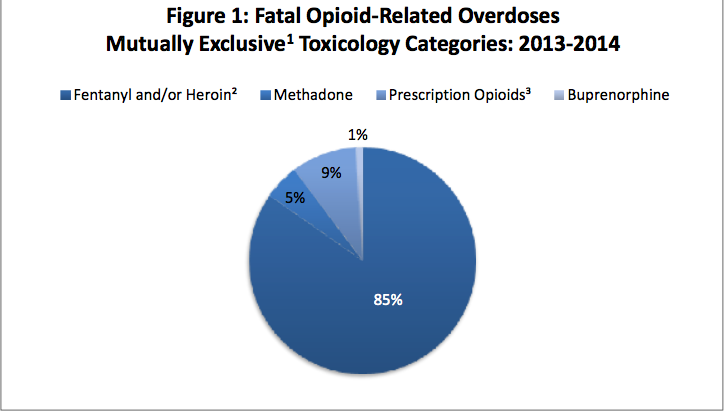
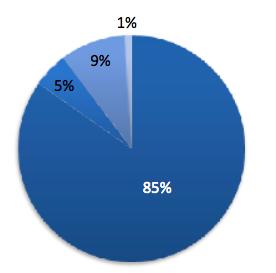
Fatal opioid-related overdoses in Massachusetts, 2013-14. Massachusetts Department of Health
From the pie chart above, it is apparent that overdose deaths from prescription drugs (9%) were dwarfed by those from heroin, fentanyl, or a mixture of both (85%). So, when a headlines says "There were 100 opioid overdose deaths last week," what it really means is that nine deaths were a result of pills, and 85 from heroin/fentanyl (1).
Perhaps more intriguing is a table from the same report, which analyzed the prescription opioid consumption patterns of the people who died from any narcotic over a four-year period:
The table shows the percent of people who died (2013-2016) from opioid overdoses, and how often they had filled a prescription for a legal opioid (Vicodin, Percocet, etc) at different time intervals over the course of the study. Of those who had confirmed or suspected heroin and/or fentanyl in their blood (red box) at the time of death, only 10-17% had filled a legal prescription for pills within one month of death. During the six months (blue box) before death before, 23-30 percent had filled prescriptions fof the pills. However, o er the course of the four year study, about two-thirds of the decedents had done so.
These data indicate that: 1) most of the people who died during the four-year interval used legal opioids at least once, but few did so within one month of death; and 2) the extensive change in prescription use over time strongly suggests that people who were pill users in 2013 were much more likely to be heroin users in 2106, but were no longer pill users. In other words, drug abusers switched from pills to injectable narcotics during a time when the pills were becoming more difficult to obtain. This is consistent with the trend shown in the OxyContin graph above.
This is, in fact, one of the findings of the Massachusetts Department of Public Health:
Individuals who died from opioid‐ related overdoses are much more likely to have an illegally‐obtained substance (i.e., not Schedule II‐III opioid) present in post‐mortem toxicology
In other words, the people who are taking pills are responsible for only a small fraction of the overdose deaths. It is the people who have switched from pills to more dangerous narcotics who are the primary victims. It is not unreasonable to at least wonder whether tighter restrictions on legal prescriptions resulted in an increase in overdose deaths instead of the desired decrease.
A similar trend can be seen nationwide, according to NIH data. This is rather intriguing.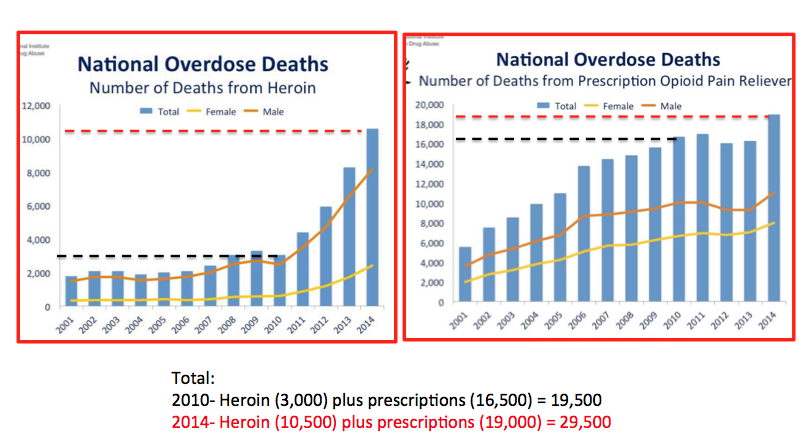
Source: Adapted from National Institute on Drug Abuse.
The graph on the left shows the number of heroin overdose deaths from 2001-2014; the one on the right, the number of prescription opioid deaths. If we focus on the period between 2010 (black hatched line) and 2014 (red)—the time during which the crackdown on prescription opioids began to accelerate—heroin deaths, which had been more or less stable for the 10 previous years, more than tripled—from 3,000 to 10,500. Additionally, during that same time, overdose deaths from prescription opioids (graph on right) also increased from 16,500 to 19,000. So, during this time there was a net increase in total opioid deaths during this time, with 75% of the increase attributable to overdoses of heroin users who made the switch from prescription pills.
Although not definitive, these graphs when taken together suggest that not only did the crackdown on opioid prescriptions failed to stop overdose deaths during that time, but may have even increased them. Furthermore, these data do not reflect what has happened since 2015, when the CDC's "voluntary" guidelines were implemented, so this effect will most likely be magnified.
Although the question "have we been helped or hurt by the drastic change in opioid prescribing practices?" remains unanswered, and may remain so for quite some time, it is difficult to picture the images of bodies in the street with needles still stuck in their arms, and the two bullet holes in Denny Peck's head, and not at least question the CDC response to an already-bad problem. Did we make things better or worse? Are we prepared as a society to accept guaranteed suffering for some to protect others from addiction?
Tough question, but David Hendry has his own thoughts, and they are not optimistic: "The callous decision-makers exemplify the words of Francois de La Rochefoucauld: 'We all have enough strength to endure the misfortunes of others."'
As usual, simple answers to complex problems rarely work, something many of us will eventually find out the hard way. The painful way.
Notes:
(1) Extrapolated from Massachusetts data.



