One of the more controversial moves during the administration of former New York City Mayor Michael Bloomberg was the banning of synthetic trans-fatty acids (TFAs) from NYC eateries (in 2007) because of concern about deleterious influences on blood cholesterol. Other New York State counties, mostly surrounding the NYC area, followed suit, and that eventually led the FDA's ban of partially hydrogenated oils (PHOs — the sources of synthetic TFAs) which is set to take effect in 2018. Synthetic TFAs can still be used in bakery products. e.g. breads. cakes, pies and pastries as well as other foods in which a solid or semi-solid type of fat was desired but most other products have voluntarily stopped using them.
Dr. Eric J. Brandt from the Yale University Medical School and colleagues investigated whether or not these bans had had any effect on the incidence of cardiovascular disease since their inception. They examined data at the county level in NYS — comparing the occurrence of a combination of heart attack (myocardial infarction - MI) and stroke as well as of each individually, in counties that did and did not restrict the use of TFAs. Their report was published in the Journal of the American Medical Association.
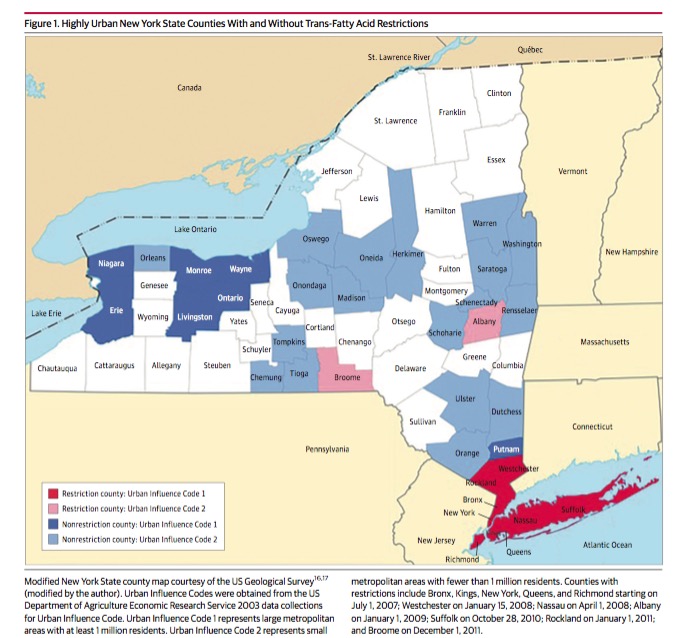
The investigators used data on all hospital admissions for MI and stroke from 2002 to 2013, sourced from the NYS Department of Public Health. The counties with TFA restrictions tended to be those with higher urban character, so for comparison they only used non-restricted counties with similar urban sizes, i.e. similar Urban Influence Codes (see diagram). Most of the UIC 1 counties with restrictions (dark red) were in southern NYS, while most of the UIC1 unrestricted counties (dark blue) were in the western part of the state
The investigators then examined hospital admissions for MI and stroke combined and individually, from before the restrictions were applied in the restricted counties, and again after the restrictions had been applied. The idea was that the admission rates in both groups would change over time. In all the counties, that could be due to any number of factors, e.g. changes in drugs used, but the differences between the restricted and unrestricted counties' admission rates for those endpoints would supposedly be due to restrictions of TFAs.
And indeed they did see a difference in the changes in admission rates between 2002 (well before any restrictions were applied) and in all restricted counties three or more years after restrictions were applied (until the end of 2013). They found that in all counties, the rates of admission for the designated endpoints fell in a similar manner between 2002 and 2006.over the studied period. But the rate of admission for the combination of heart attacks and stroke fell significantly more in the restricted counties between 2006 and 2013 than in the others. The same was true for heart attacks alone. This analysis was thus of the size of the differences at the end of the study period compared to the differences at the beginning. My colleague, Dr. Chuck Dinerstein has written a commentary on the details of such a comparison, which can be seen here.
The confounders
At first glance, these results provide support for the hypothesis that TFAs are causally related to the risk of heart attacks and stroke, but further study is clearly necessary, since the demographics and many lifestyle characteristics likely differed.
For example, it was difficult to account for real differences between people who lived in NYC and those who lived in far western New York counties when recall bias is an obvious problem.
Although the authors attempted to account for such differences statistically in the current study, it would be more accurate to actually see what effect, if any, the TFA restrictions had on different populations with different risk factors.

