Genetics plays a role in almost any conceivable characteristic, not just the obvious ones like eye color and height. Indeed, genetics plays a role in susceptibility to infectious disease, mental illness, and even personality traits.
Despite this being a widely acknowledged fact, the role of genetics is downplayed or outright ignored in certain situations that society finds uncomfortable. Most notably, we shy away from discussing the role of genetics when it comes to biological differences between the races and genders. Differences there are often blamed on social factors, such as discrimination, rather than biological ones. We do this, however, at our own peril.
To be sure, environmental and social factors (such as socioeconomic conditions, lifestyle choices, and adequate access to healthcare) play an important role in disease outcomes. But, genetics often does, too. A new review published in Trends in Cancer underscores this point by demonstrating that African-Americans appear to have a unique genetic susceptibility to cancer, both in terms of acquiring the disease and dying from it.
The authors discuss various lines of evidence to make their case. For instance, though Hispanic Americans share many of the same socioeconomic conditions as black Americans, Hispanics have better cancer outcomes. Additionally, when factors such as lifestyle, socioeconomic conditions, and access to healthcare are controlled, black Americans are likelier to be diagnosed with and die from cancer than whites.
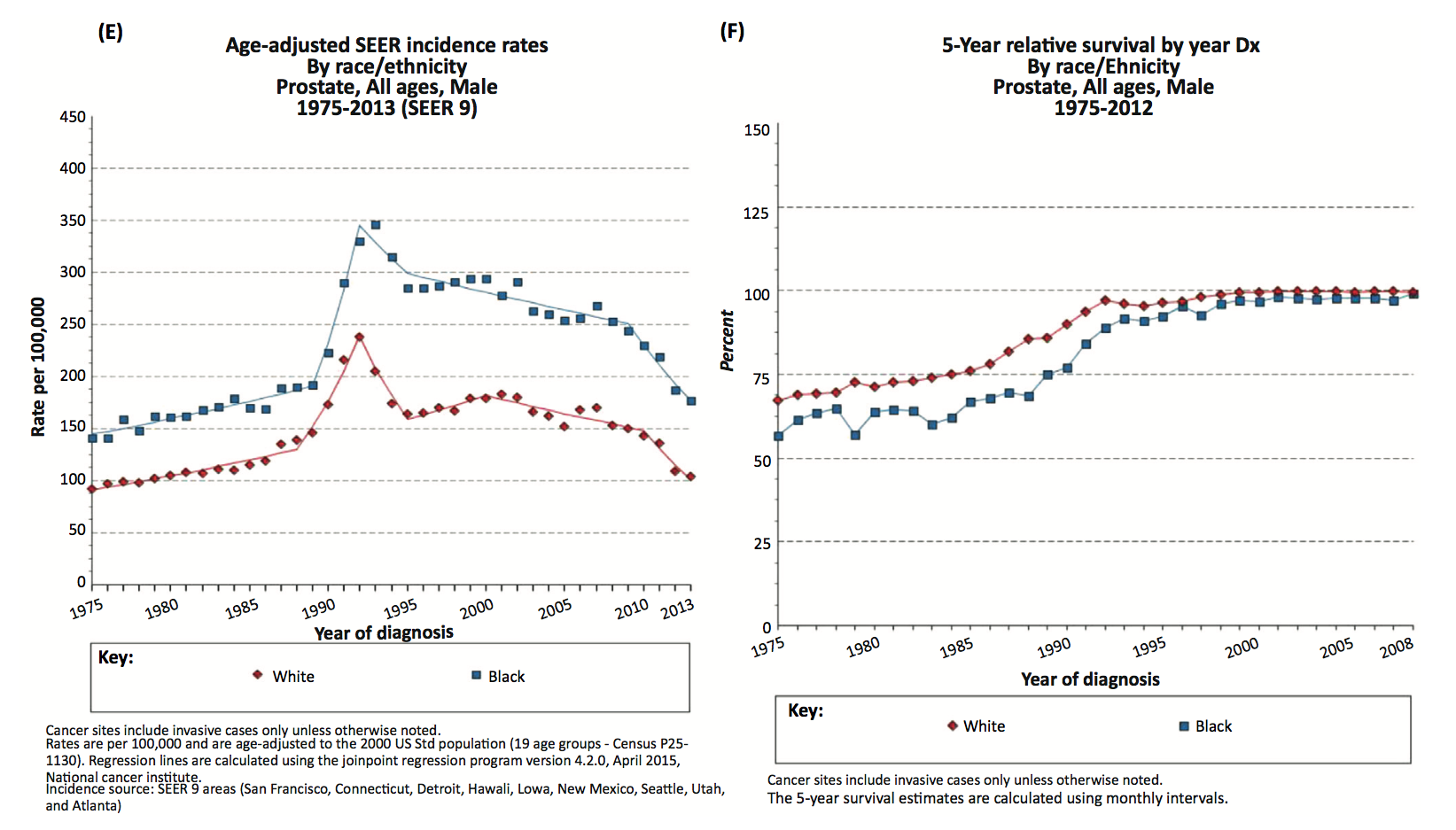
A particularly compelling argument compares the incidence of prostate cancer (i.e., the number of new cases) among white and black men with five-year survival rates. Today, both white and black men have roughly the same outcome (nearly 100% survival five years after diagnosis), but black men are far more likely to be diagnosed with the disease in the first place. This strongly suggests that, for prostate cancer at least, something other than healthcare access is causing the higher rate of cancer.
Because, as mentioned earlier, black Americans have worse cancer outcomes than whites even after various confounders are controlled, this would indicate that genetics plays a role in the disparity. What sort of genes may be involved?
The authors propose that gene variants (called alleles) linked to obesity and chronic inflammation may be to blame. Roughly 14 to 20% of cancer deaths may be related to obesity, and obesity is more prevalent among African-Americans than among whites. (Hispanics are also more obese than whites but are not as susceptible to obesity-related cancers. This could be due to genetic and/or dietary factors.)
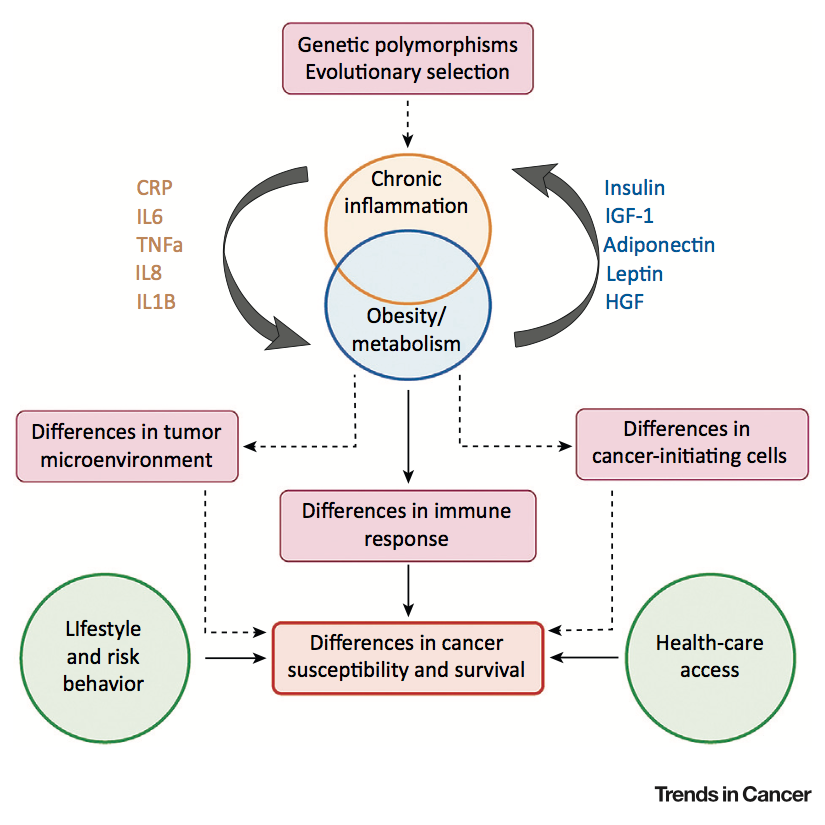 Similarly, 15 to 20% of cancers may be due to infections and inflammation. Once again, compared with other races, blacks have higher levels of pro-inflammatory proteins in their blood. Additionally, African-Americans' innate immune systems -- which play a role in cancer -- are genetically distinct from other races.
Similarly, 15 to 20% of cancers may be due to infections and inflammation. Once again, compared with other races, blacks have higher levels of pro-inflammatory proteins in their blood. Additionally, African-Americans' innate immune systems -- which play a role in cancer -- are genetically distinct from other races.
Combined, the authors' argument leads to the conclusion that, contrary to popular wisdom, disparities in cancer-related health outcomes among the races may have a strong biological component rather than just a socioeconomic or lifestyle component. With this in mind, they developed a model of all the various factors that likely play a role in cancer outcomes. (See figure on right.)
Of course, acknowledging genetic factors in cancer outcomes is not an excuse to ignore the role of socioeconomic factors. However, to beat cancer, we must understand all of its causes -- even the ones that make us uncomfortable.
Source: Berna C. Özdemir, Gian-Paolo Dotto. "Racial Differences in Cancer Susceptibility and Survival: More Than the Color of the Skin?" Trends in Cancer 3 (3): 181-197. Published: March 2017. doi: 10.1016/j.trecan.2017.02.002