
Bariatric surgery, as we've noted before, is currently the most effective way to deal with extreme obesity. But just having the surgery doesn't guarantee success — the subject must still exercise some degree of dietary discipline to obtain the most benefit from the procedure, as demonstrated by a report published in the American Journal of Clinical Nutrition.
Dr. Noora Kanerva from the University of Gothenburg, Gothenburg, Sweden, and colleagues analyzed data from the Swedish Obesity Study (SOS), a more than 30-year investigation comparing bariatric surgery with conventional treatments for obesity. In particular, they were interested in learning whether the short-term dietary changes a person made after bariatric surgery (i.e. in the first six months) might be predictive of the long-term (10 years) success of the procedures. In part, their interest stemmed from the observation that about “20-30 percent of obese patients do not achieve successful weight outcomes after bariatric surgery.” Their concept was that the ability to adapt to the changes necessary for weight loss after bariatric surgery would be predictive of long-term weight loss success.
Individuals’ weight, height and waist circumference were measured at periodic interview sessions, and food intake and activity levels were self-reported. Data from about 2,000 subjects of the SOS were included in this analysis. Criteria for participation included a BMI of over 34 for men and over 38 for women and ages of 37-60 years. Baseline data were obtained four weeks prior to surgery.
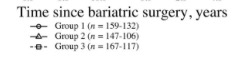
Changes from baseline values were assessed at six months and periodically until ten years post-surgery. Based on changes from baseline, the respondents’ energy intake reductions were divided into three groups: group 1 had the smallest reduction (300 kcal), group 2 an intermediate reduction, and group 3 the largest reduction (2500 kcal).
By ten years post-surgery, the investigators found that men lost an average of 15 percent of initial body weight, while women lost about 17 percent. In addition, they found that the percent of weight loss at ten years post-surgery tracked with the degree of reduction in energy intake at six months, as shown below.

Thus they concluded that early weight loss was indeed predictive of the long-term success of surgery-induced reduction. While their conclusion is logical, there are weaknesses in the design of this study. First, the type of surgery varied among individuals — most had had vertical gastric banding procedures, while others had another form of gastric banding and yet a third group had gastric bypass surgery. It isn’t clear whether the success at ten years was influenced by the type of surgery as well as by the early reduction in energy intake. Further, surgical procedures change with time — for example, more recently the proportion of bariatric procedures performed via laparoscope is much higher than it was when this study began. And of course, the fact that food intake was self-reported also leaves some room for error.
Taking such caveats into account, it is important to note the variability of the surgical result with respect to energy intake and weight loss. These data suggest that more education would be helpful in impression on surgical candidates that their actions in changing their behavior will determine the relative success of the procedure. The surgery can’t do it alone.



