OK, the headline is a bit like clickbait, I do not believe Ivermectin is useful, but I could be wrong. (Did I just say that?) A new study demonstrates how a rush to publish, (and possibly treat) may have resulted in poorly designed studies where a quiet signal is lost in an abundance of noise.
While effective vaccines are an incredibly important part of the COVID-19 solution, none are completely effective, and so we do need anti-virals to reduce the severity of those who become infected. There have been many candidates that have come and gone, most recently Ivermectin as we have written. A new study published in PLOS Medicine looks at the design of these studies and suggests that in the urgency to treat, we did not craft well-designed studies to demonstrate efficacy.
“An antiviral drug would be useful in limiting the severity of disease in people who are not vaccinated or contract a variant not covered by a particular vaccine.” Josh Bloom, Ph.D
The researchers used a computer model of COVID-19 in which varying viral loads in a population would result in differing rates of infectivity – it is a reasonable approximation of real-world COVID-19 experience. They manipulated the viral loads within their “population,” its heterogeneity, and the time that an anti-viral was given – at the first sign of symptoms or perhaps a few days later when you were sufficiently ill to seek medical attention.
The model made use of real data on the changing viral load in 30 patients assessed with PCR daily. Viral loads were “quantified” based on calculating the number of cycles necessary for amplification before the PCR test became positive (fewer cycles, higher loads). The emphasis on viral load was because of the underlying assumption that viral load equates to disease severity. By the way, this is some of the first data I have seen on those dynamics.
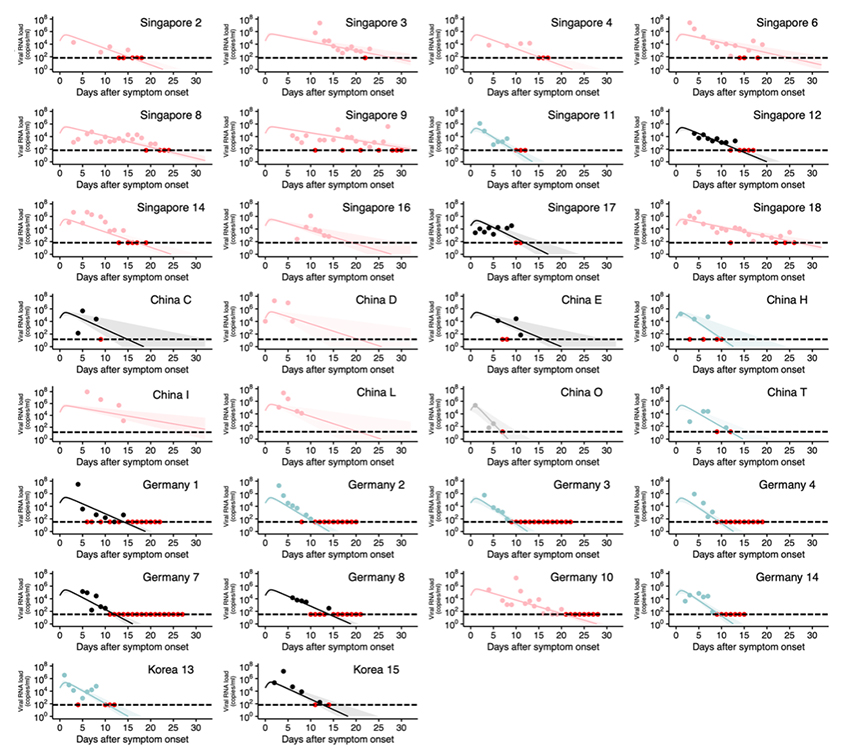
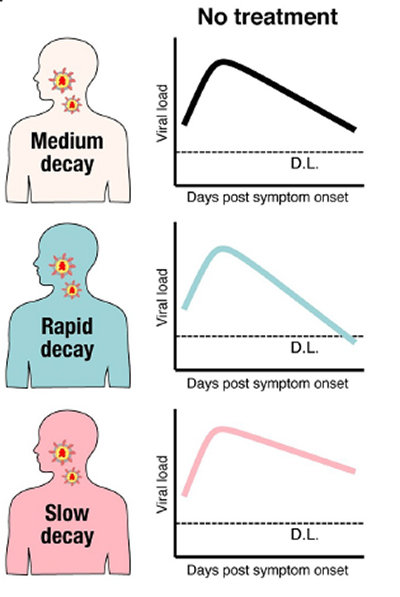
As the graphic demonstrates, the viral load increases quite quickly and then “decays” over time. A statistical analysis of the data showed that the viral load’s trajectory, the shape of those curves, were only minimally impacted by the rise. The greatest variation in viral load was in the decay phase, as our immune system neutralized COVID-19. That used that analysis to describe three groups within the population-based upon decay rates of the viral load.
The model found that
 Use of an anti-viral after the viral peak was reached, even one 99% effective in inhibiting viral replication, had no impact upon the trajectory – there were diminishing virions to inhibit, too late.
Use of an anti-viral after the viral peak was reached, even one 99% effective in inhibiting viral replication, had no impact upon the trajectory – there were diminishing virions to inhibit, too late. - An anti-viral with 50% inhibitory efficacy had no effect because it left too many virions able to multiple – too little and too late.
- An efficacious response to anti-virals was only found when given within 12 hours of the onset of symptoms; waiting 5 days could not alter COVID-19’s trajectory – once again, too late.
The graphic below this paragraph sums the model’s results. An anti-viral will reduce viral shedding, taken as the measure of disease severity, only if given very early, within 12 hours of initial symptoms, with maybe an outer limit of 48 hours. While the analogy is not perfectly matched, it is the same time course we expect with Tami-Flu, given early is reduces the time course of the flu.
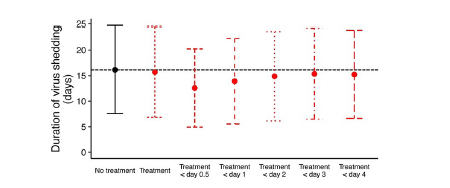 When the researchers looked at 110 studies registered with ClincalTrials.gov, only 15% had an inclusion or exclusion criteria related to the onset of symptoms. The average time to initiate an anti-viral was slightly more than seven days, far beyond any efficacy these medications might offer. The plethora of observational studies prompted by the pandemic have a fatal design flaw; they did not control the initiation of treatment. As a result, the number of participants needed to show a statistically significant effect would be about 11,000. If a study were restricted to those treated within 24 hours, the necessary number of participants would decrease to 450.
When the researchers looked at 110 studies registered with ClincalTrials.gov, only 15% had an inclusion or exclusion criteria related to the onset of symptoms. The average time to initiate an anti-viral was slightly more than seven days, far beyond any efficacy these medications might offer. The plethora of observational studies prompted by the pandemic have a fatal design flaw; they did not control the initiation of treatment. As a result, the number of participants needed to show a statistically significant effect would be about 11,000. If a study were restricted to those treated within 24 hours, the necessary number of participants would decrease to 450.
The actual numbers are not important in moving forward. To either promote the use or drive a stake into the heart of the Ivermectins of the world, we need a well-designed study. The work done in the heat and urgency of the COVID-19 moment will not give us any useful answers no matter how we cast about. Science is self-correcting. We can put the use of the anti-virals to a better test if we take a few moments to design better studies. Is it time for an RCT for Ivermectin?
Source Detection of significant antiviral drug effects on COVID-19 with reasonable sample sizes in randomized controlled trials: A modeling study combined with clinical data PLOS Medicine DOI: 10.1371/journal.pmed.1003660

