It has been sixty years since the Concert for Bangladesh; It is doubtful that this low-income country, with half the population and 1/66th the size of the US, has had as much coverage in the media as now, with a report on the efficacy of masks in fighting COVID-19. It is a well-thought-out, performed, and reported study and deserves better than the superficial reporting of the media and 280 character Tweets. Let me provide a deeper look.
"A randomized-trial of community-level mask promotion in rural Bangladesh during COVID-19 shows that the intervention tripled mask usage and reduced symptomatic SARS-CoV-2 infections, demonstrating that promoting community mask-wearing can improve public health.”
Let’s begin with context and intent
Bangladesh is far smaller and more densely populated, at least in its urban centers, compared with the US. More importantly, Bangladesh is poor, and like many other low and middle-income countries, has neither infrastructure nor funding for COVID-19 vaccinations. They need preventative measures that are cheap and widely available. Hence, a study of masks and social distancing is desperately necessary to provide some guidance in protecting their populations. The study is designed to help these countries. Any value in their findings for a high-income country, like the US, is nuanced – neither the mainstream nor social media have the time or inclination to go to the trouble to be nuanced, there is ad revenue, “likes,” and “re-tweets” to be earned.
“Our entire intervention was designed to be easily adopted by other NGOs or government agencies and required minimal monitoring.“
The study involved nearly 350,000 people, a number the media loves to share. But it is a study in Bangladesh’s rural community. We are talking about villages of roughly 500 people. In the US, approximately 31% of our incorporated communities are that size. 500 is also about a third of the population on the average block in New York City.
The study had two outcomes of interest; the effect of their intervention on seropositivity, the presence of antibodies to COVID—19, and wearing masks and social distancing.
Non-pharmaceutical Interventions
The why:
“In Bangladesh, a quarter of those observed in public areas in June 2020 wore masks, and only a fifth wore masks properly (covering both the nose and mouth), despite a nationwide mask mandate in effect at the time. This raises questions about how to increase mask-wearing in community settings.”
The government formally mandated mask use in late 2020, which included fines for non-compliance, “although enforcement was weak to non-existent, especially in rural areas.” That bears some similarity with our approach. They provided, as part of their randomization, cloth or surgical masks. Cloth masks were a bit more expensive at $0.50 each with a filtration efficacy of 37% against particles in the range of our airborne concerns; surgical masks were far more effective at 95%, and their cost was much less $0.13.
The researchers spent time developing and then describing how they developed their intervention. In addition to filtration measures, they consider behavioral economics, marketing, reminding, and communication studies. Here is the intervention
“Intervention arms received free masks, information on the importance of masking, role modeling by community leaders, and in-person reminders for 8 weeks.” [Emphasis added]
Those role models included the imams who discussed the importance of mask-wearing at Friday prayers. Our role-modeling by community leaders is in many places non-existent, as Governors Newsom and Abbott, among others, have demonstrated.
The media has pointed out that most of the data reflected outdoor locations. In these small villages, the mosques are the most important indoor community meetings and potential community spread. But those areas were monitored just like the outdoor communal areas, i.e., marketplaces. The other caveat that the media point to is that compliance was measured only once a week. While that is true, the surveillance ran from 9 AM to 7 PM – I think that is a reasonable sampling. And while indoor or outdoor matters discussing seropositivity, it has little meaning when talking about compliance. The only caveat that the media never mentioned was that wearing a mask is a visible virtue signal “where social norms are expected to be important.” Like a Tesla signals your concern about fossil fuels.
Those interventions:
- “…increased proper mask-wearing from 13.3% in control villages to 42.3% in treatment villages. This tripling of mask usage was sustained during the intervention period and two weeks after.” Five months later, that tripling had declined but was still 50% more than the control villages.
- “Physical distancing increased from 24.1% in control villages to 29.2% in treatment villages. This 5% absolute increase is not large and is tempered by the absence of “physical distancing practiced in any mosque, in either treatment or control villages, probably as a result of the strong religious norm of standing shoulder-to-shoulder when praying.” In the marketplace, physical distancing was a bit greater, 7.4%.
- Mask-wearing increased in the mosques by roughly 37% - the only indoor site to be considered and where the greatest transmission might occur. In the outdoor locations, mask-wearing increased by 25% or more.
- “Contrary to concerns that mask-wearing would promote risk compensation, we did not find evidence that our intervention decreases distancing behavior.” Masks and social distancing were complimentary behaviors, not substitutes. The Bangladeshi villages understood that you need to apply multiple protective layers.
But here is a finding that none of the media mentioned
“…combining mask distribution, role-modeling, and active mask promotion – rather than mask distribution and role-modeling alone – seems critical to achieving the full effect. Our trial results also highlight many factors that appear inessential: we find no evidence that public commitments, village-level incentives, text messages, altruistic messaging, or verbal commitments change mask-wearing behavior.”
Preventing COVID-19 by using non-pharmaceutical interventions cannot be left to messaging. If you wish to use a war metaphor, instituting preventive measures is hand-to-hand combat, something we are reluctant to do. We prefer to speak at a distance rather than act up close and personal.
Seropositivity measures
The why:
“Our trial is therefore designed to track the fraction of individuals who are both symptomatic and seropositive. We chose this as our primary outcome for two reasons: first, the goal of public health policy is ultimately to prevent symptomatic infections (even if preventing asymptomatic infections is instrumentally important in achieving that goal). Second, because symptomatic individuals are far more likely to be seropositive, powering for this outcome required conducting an order of magnitude fewer costly blood tests.”
Let us begin with the bottom-line result.
“The proportion of individuals with COVID-like symptoms was 7.62% (N=13,273) in the intervention arm and 8.62% (N=13,893) in the control arm.”
For those who wish to minimize the finding, this is an absolute reduction of 1%. For those who want to maximize the result, this is a relative reduction of 10%. Pick your number, but consider an important caveat, only 40% of the symptomatic were tested. As the researchers report, “Because these numbers omit non-consenters, it is likely that the true rates of symptomatic seroprevalence are substantially higher (perhaps by 2.5 times, if non-consenters have similar seroprevalence to consenters).”
The intent of the research was a low-cost, easy preventative measure for low and middle-income countries where vaccines, the most effective preventive measures, are not available—framed that way, their intervention increased mask use by 30% and reduced symptomatic COVID by 10%. I call that a win; what do you think?
This graphic has been featured widely.
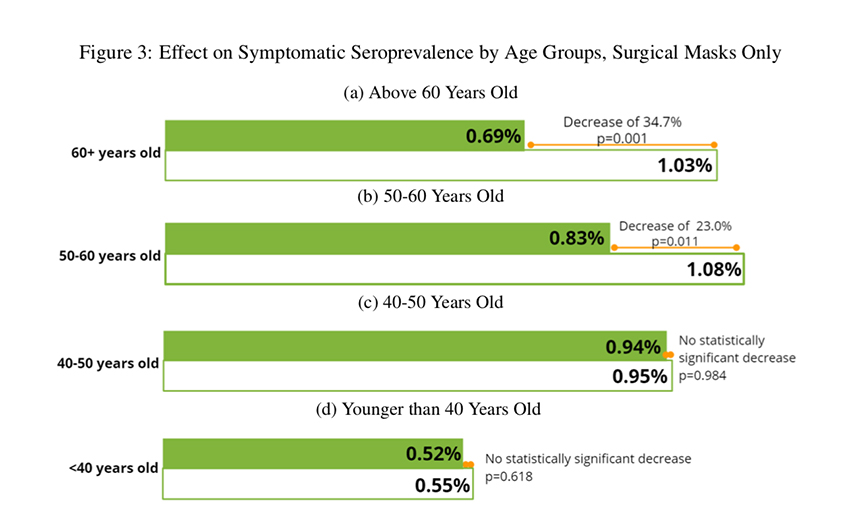
Much has been made about the lack of effect on those under 50. But consider this. The study involved the alpha variant, which we know found few susceptibles in that age group – Delta is different. But among the susceptible, the over 60 crowd, the decline was nearly 35% in seropositivity. Masks reduce transmission to the most vulnerable, the elderly; isn’t that the goal?
Policy-making and cost
The researchers presented their data to “the World Health Organization, the World Bank, and the National Council of Applied Economic Research in Delhi, India” – an audience of experts. But before their presentation, they asked the experts what they anticipated were the findings. Would you be surprised with the following?
- “Policy-makers makers believed that in-person reinforcement would have no additional impact, despite our piloting suggesting it is the single most important element of our intervention.”
- “64% of respondents predicted that physical distancing would either decrease or remain unchanged as a result of the mask-promotion interventions, when in fact, it increased.”
- “68% of respondents believed that text messages would help (they didn’t).”
- “62% of respondents believed that incentives for village-leaders would help (they didn’t.”
- 77% of respondents believed that verbal commitments or commitments made using signs on one’s door would increase mask-wearing (they didn’t).”
“…only a tiny fraction of policy-makers correctly predicted the impact of our core intervention on mask-wearing and physical distancing.”
The researchers estimated the cost of this intervention as $1.50 per person, a bargain. For those who relish metrics, to save one life, there is a total cost of $10,000 to $25,000 – “This is considerably lower than the value of a statistical life in Bangladesh ($205,000).” For comparison, to save one life with open heart surgery for coronary artery disease costs $3,775,000.
“In summary, we found that mask distribution, role modeling, and promotion in a LMIC setting increased mask-wearing and physical distancing, leading to lower illness, particularly in older adults. We find stronger support for the use of surgical masks than cloth masks to prevent COVID- 19.”
You can find my colleagues insightful comments on the media's reporting here.
Source: The Impact of Community Masking on COVID-19: A Cluster-Randomized Trial in Bangladesh

