Although dermatology may not automatically command the respect of other disciplines such as oncology, Drs. Henry Miller and Renata H. Mullen explain why dermatology is one of modern medicine’s most complex and fascinating specialties.
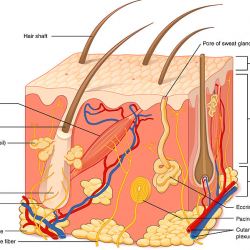
If you were to ask people who have been to a dermatologist what those medical specialists do, many would probably say something like, “they give you cream for an itchy rash or acne,” or “freeze spots on your skin to remove them.” But the diagnosis and treatment of diseases of the skin — the human body’s largest organ -- is both misunderstood and underrated.
The reality is that skin diseases are important because they are common, impose a huge economic and psychological burden on patients, and can be serious, even deadly. A corollary is that regular dermatological checkups are a good investment of time and healthcare resources. Several years ago, one American in four sought treatment for at least one skin ailment, and the average person was treated for 1.6 skin diseases. Nearly half of Americans over age 65 have skin diseases, with an average of 2.2 each. Treatment of skin disorders accounted for $75 billion in medical, preventative and prescription and non-prescription drug costs.
Because of the difficulties in maintaining personal hygiene, dermatologic diseases are the scourge of military campaigns. In the southern Pacific during World War II, some 20% of soldiers seeking medical attention suffered from a “dermatologic process,” and during the Vietnam War, 2.2% of all military outpatients had a skin disease. In Operation Desert Storm in the Persian Gulf, the frequency was 13.9%.
Skin diseases are often serious, and many can actually be fatal. The threat of malignant melanoma is well-known, but non-melanoma skin cancer also causes or contributes to significant morbidity and mortality. Moreover, common skin diseases such as psoriasis are associated with serious medical conditions including heart disease and diabetes. Infections are another common problem.
In spite of the importance and frequency of skin diseases, there are many myths and misconceptions about them and the dermatologists who diagnose and treat them. For example:
• Dermatologists don't only do cosmetic procedures. They deal primarily with skin disorders, such as psoriasis, allergic and intrinsic eczema, lupus, acne, and hair and nail disorders. They also diagnose skin cancer, and some specialize in the surgical removal of difficult skin cancers.
• Many infectious and internal diseases have skin signs. These include the fingernail pigmentation that indicates arsenic poisoning; the dry, scaly skin of hypothyroidism; the yellowing of the skin (jaundice) in liver failure; rashes that signify underlying systemic disease -- for example, the butterfly-shaped facial rash that is found in lupus; the red bumps over the skin of the joints typical of dermatomyositis, a rare inflammatory disease of the skin and muscles; and the soft-tissue benign tumors that can indicate Cowden’s syndrome, which predisposes to breast, thyroid and uterine cancers; and the pinpoint red spots that can be a sign of vasculitis, septicemia, low platelet counts or leukemia.
• Dermatologists often make the initial diagnosis of sexually-transmitted diseases, all of which have skin manifestations.
• There are actually dermatologic emergencies, including sudden blistering of the skin; and differentiating whether a suddenly-appearing rash is due to an infection, reaction to a drug, or an autoimmune disease (such as lupus).
• Many skin diseases have important implications for quality of life. Patients with serious illnesses — diabetes or cardiac or renal disease, for example --show no outward signs and can move through society invisibly, but patients with certain skin diseases have daily encounters with strangers staring, being repulsed by the sight, or thinking they might be contagious. Moreover, patients with visible skin diseases often feel unattractive and stigmatized. (Think of your worst bad-hair day, multiply by ten, and that would be your lot, all day, every day.) Having an itchy, scaly rash can significantly decrease self-esteem and interfere with interpersonal relationships. There is a high rate of depression and anxiety in patients with many chronic skin disorders, including psoriasis, vitiligo, eczema and acne.
• Melanoma, a potentially deadly form of skin cancer, is increasing at the fastest rate of all cancers in the United States. Many people believe that it develops only in sun-exposed areas, has to be raised, develops only in a mole, and occurs only in light skinned people and the elderly, but none of that is correct. In fact, melanoma can occur even in teenagers, may occur on skin that does not have any moles, may be completely flat, develop on any part of the body, and not cause any symptoms. Melanoma can therefore completely fly under the radar unless you look for it.
Some people think the practice of dermatology is boring. In fact, you get to see wild and even macabre things:
• A newly formed cyst on the scalp from which you pull out a couple of large botfly larvae (acquired in the rainforest in South America);
• An elderly woman comes in with a rapidly enlarging “mole” on the back, which turns out to be a tick, engorged with blood;
• A consultation request comes from the cardiology department to diagnose a rash in an elderly man. Upon closer examination, the rash is moving, and you find that it consists of live lice on his chest hair;
• Old embedded objects, from glass shards to shrapnel, may work their way out through the skin years, or even decades, after they entered.
So, dermatology is far more than skin deep. But that leaves unanswered the question of what dermatologists look for and do during an exam. One of the key factors in a skin exam is to allow the dermatologist to check the patient’s entire skin, including the areas that are never exposed to the sun. This can uncover hidden skin cancers as well as offer clues to diagnose rashes and other skin findings more precisely.
When examining moles and other spots, a dermatologist will often look for the “ugly duckling”, meaning a spot that looks different from a patient’s other spots. This is then checked with a dermatoscope, an instrument that allows the dermatologist to see what structures are deeper in the skin based on reflected light.
Dermoscopy has revolutionized the field of dermatology and has allowed much more precise diagnosis of a lesion than what was previously possible with the naked eye. This has significantly improved the decision on whether or not to biopsy a lesion. It has also improved the ability to recognize melanomas early, while they are still easily treatable.
In spite of its image, dermatology is one of modern medicine’s most complex and fascinating specialties.
Renata H. Mullen is a physician who practices dermatology in Palo Alto, California. Henry I. Miller, a physician and molecular biologist, was a research associate at the National Institutes of Health and the founding director of the FDA’s Office of Biotechnology.