A group at Sloan Kettering is proposing the use of certain types of chemotherapy drugs to treat SARS-CoV-2 infection. One cannot help thinking of the old adage about what everything looks like when you only have a hammer.
The race to discover anti-COVID drugs, just like the race to discover any drugs, has been long (1) and frustrating. Remdesivir, the direct-acting antiviral drug that garnered much attention a year ago, has been disappointing. Merck and Ridgeback's molnupiravir, aka EIDD-2801, which was described in March by Derek Lowe in his In the Pipeline series as the "Last of the Small-Molecule Coronavirus Hopes?" is progressing into Phase 3 trials and is said to be doing well. Pfizer just began a Phase 2/3 trial of PF-07321332, a protease inhibitor plus ritonavir (2). Some very potent (single-digit nanomolar) drugs that target the SARS-CoV-2 main protease MPRO have been reported.
Molnupiravir has recently progressed to Phase III clinical trials and early results from previous trials seem to show it has promise for treating mild to moderate cases of COVID. These results are apparently so encouraging that the US Dept of Health and Human Services has promised to pay $1.2 billion for around 1.7 million courses of molnupiravir should they receive FDA approval. Initial skepticism over the potential for toxicity remains for some in the field, due to the mechanism of action - lethal mutagenesis - but to date, the data seems to show it is safe, thus this may provide another small molecule drug to help fight the pandemic.
Prof. Kathie Seley-Radtke, Ph.D., Professor, Chemistry & Biochemistry, University of Maryland, Baltimore County
Some of the drugs proposed as potential COVID drugs have been a bit of a stretch and here's another stretch – chemotherapy drugs to treat COVID. A new JAMA Oncology paper asks whether a subset of chemo drugs that are associated with lower expression of the angiotensin-converting enzyme 2 (ACE2) might have an impact on SARS-CoV-2 infection since ACE2 is the binding site of the coronavirus spike protein.
Michael B. Foote, M.D., and colleagues at Sloan Kettering Cancer Center identified a cohort of 1701 patients who were undergoing chemotherapy for a variety of cancers. All were checked for COVID status. Ninety-one of the drugs being used were associated with downregulation of the ACE2 gene and, for example, inhibitors of mTOR (mammalian target of rapamycin) and PI3K (phosphoinositide 3-kinases) as well as antimetabolites – drugs such as 5-fluorouracil and methotrexate that inhibit DNA synthesis and cell division.
Of this group, 235 patients (12.6% of the cohort) had been given one of eight drugs.
- Everolimus, temsirolimus, alpelisib (mTOR/PI3K)
- Decitabine, gemcitabine (antimetabolites)
- Cabazitaxel (antimitotic)
- Dasatinib, crizotinib (tyrosine kinase inhibitors)
The results
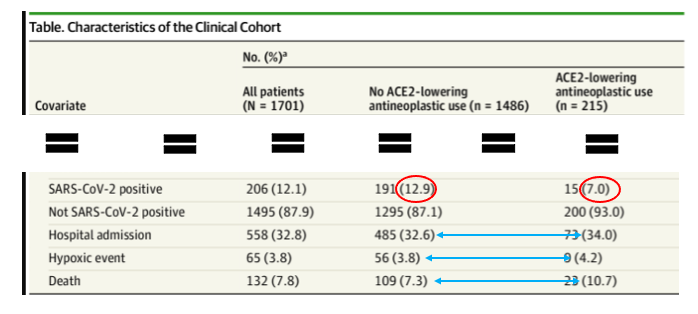
Original table: Foote, MD, et. al., JAMA Oncol. Published online August 19, 2021. doi:10.1001/jamaoncol.2021.3585
"Patients who received a potential ACE2-lowering antineoplastic exhibited a statistically significantly reduced SARS-CoV-2 positivity rate of 7.0% compared with 12.9% in patients who received other antineoplastic therapies."
What does this mean? Did cancer patients who received chemo that lowered ACE2 receptor regulation fare about two times better than patients who received other types of chemo? The positivity rates (red oval) seem to show a significant difference between the groups. On the other hand, the rates of hospitalization and hypoxic events were the same in both groups, while the death rate in the ACE2-lowering group was higher (blue arrows). So, it is difficult to see any obvious advantage in ACE2-lowering chemo drugs over the rest of them.
And, when you throw in the obvious downside of treating people who are ill with a serious viral infection with drugs with considerable side effects of their own, this paper strikes me as being wishful thinking as best.
NOTE
(1) Long is relative. We are less than two years into the pandemic. It took 14 years following the discovery of HIV for the first useful first direct-acting antiviral to be discovered. For hepatitis C it was 22 years.

