In our somewhat academic household, “solving differential equations” was a euphemism for tackling a challenging intellectual problem with an uncertain outcome. Pinning down the health effects of air pollution exposure is one such problem.
The current regulatory mantra is:
“Air pollution is the cause and aggravating factor of many respiratory diseases like chronic obstructive pulmonary disease (COPD), asthma, and lung cancer.”
“Aggravation,” an acute response to an underlying disease, has been observed in individuals; causing a chronic condition is altogether something else. The strictest air pollution regulations have been based on differences in chronic disease rates among cities. Their underlying assumption is that a change in air quality produces a change in health. For example, the most personal air quality change, smoking cessation, has been shown to improve health and lengthen longevity. Can we say the same about imposing new air pollution controls?
Could moving from polluted West Virginia to clean Vermont magically lengthen your life?
Here I explore a differential approach: by comparing changes in mortality with changes in putative causal factors during a specified period. This “differences in differences” model may provide direct estimates of the benefits of air pollution control for both acute and chronic effects. The time frame for my exploration is roughly 1990-2000 (hereafter “previous”) vs. 2010-2020 (hereafter “current”), depending on the availability of state-level public data from the 48 contiguous states and the District of Columbia. I considered the following potentially causal factors in this proof-of-concept analysis:
- Income: median annual household income, adjusted for inflation.
- Ambient air quality: annual average concentration of fine particles (PM2.5).
- Vehicular traffic: annual vehicle miles driven per capita (VMT).
- Smoking prevalence: percentage of regular smokers, based on surveys.
- Smoking amount: annual tax-paid packs of cigarettes per capita, which could include effects from second-hand smoking.
Almost all of the extant epidemiology on chronic effects has been based on spatial gradients, assuming that if a highly polluted city has more cases than a cleaner city, after accounting for all other relevant factors like age, race, smoking, etc., pollution must be one of the reasons. However, with chronic health effects, it is difficult to ensure that all relevant factors have been adequately considered. They include descriptive persistent long-term factors like population density, socioeconomic status (however measured), green space, indoor air pollution sources, and climate, and behavioral factors like smoking habits, traffic levels, and ambient air quality.
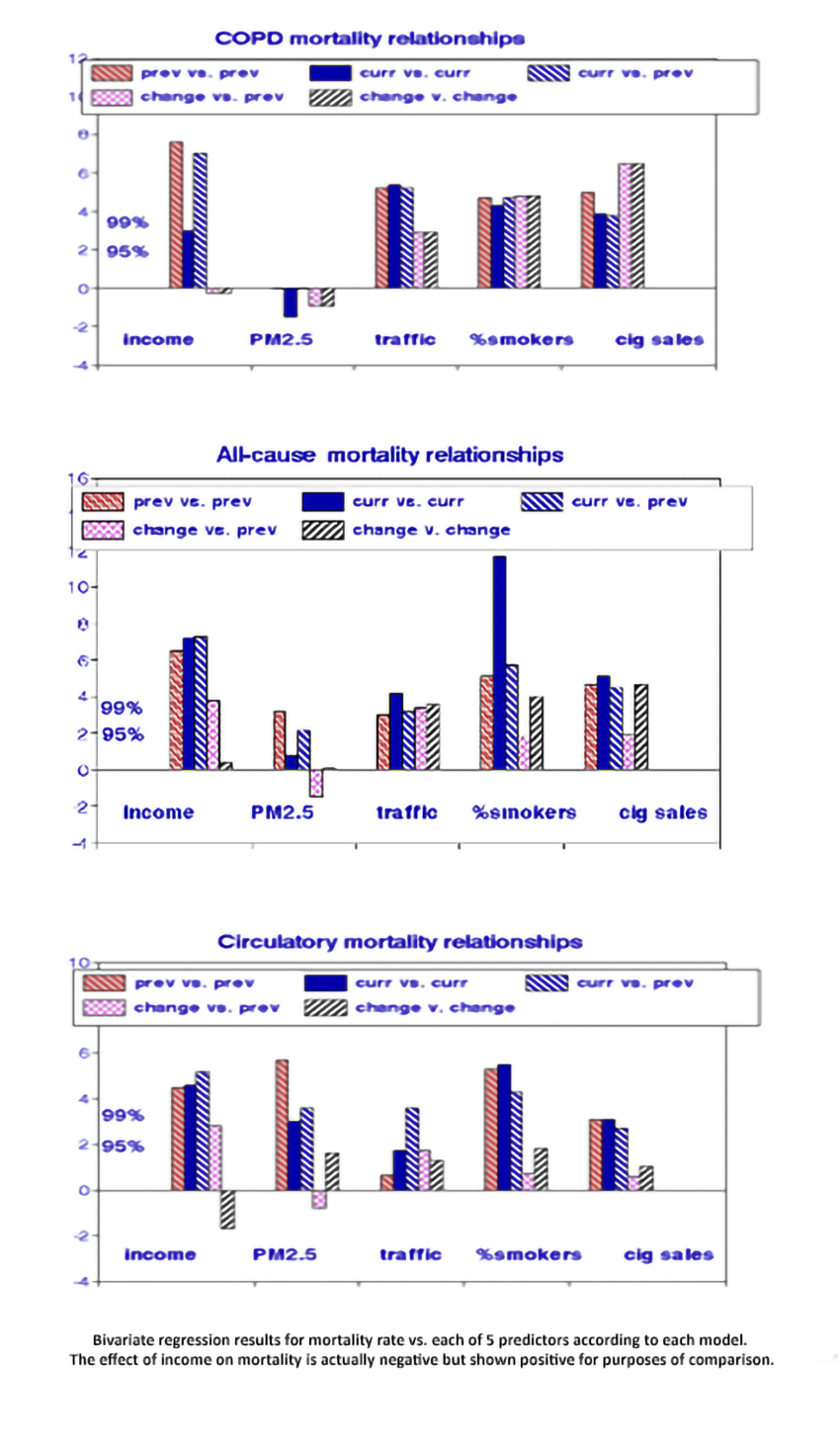
To evaluate this basic assumption, I considered three mortality groupings for each of the five regression models:
- Respiratory deaths. As the primary route of entry for air pollution, adverse health effects like chronic obstructive pulmonary disease (COPD) should appear there first.
- Circulatory deaths, including heart failure and stroke. These have often demonstrated the strong
estassociations with air pollution in regulatory studies. - All-cause deaths, including accidents, homicides, and suicides.
- Previous mortality rates vs. previous factors.
- Current mortality rates vs. current factors. This is the most prevalent epidemiological model.
- Current mortality rates vs. previous factors, considering latency effects.
- Changes in mortality rates vs. previous factors.
- Changes in mortality rates vs. changes in factors, the differential analysis of primary interest compared to the others.
Considering these five models with the five potentially causal variables and the three mortality groupings required 75 linear regressions, as shown in the graphs.
Starting with the income variable on the left, people living in high-income states appear to have lower mortality rates from all three disease groupings but getting a raise would have no effect. Moving to the right, both smoking factors indicate behavioral as well as descriptive effects; tobacco cessation or reduction was associated with reduced COPD and all-cause mortality, bolstering the evidence for causal effects. However, this was not the case with circulatory mortality, perhaps because that category was too broad. As a result, all-cause mortality must include significant contributions from other causes like cancer. PM2.5 was not significantly associated with COPD for any model and only (barely) significant for circulatory and all-cause deaths, but only with the descriptive models.
The traffic variable is more complex because of its dependence on population density. In urban states, the miles driven (VMT) tend to be higher but lower on a per-capita basis because of the higher population densities. Rural states now tend to have higher COPD and all-cause mortality levels, making associations with VMT significantly positive. The percent change in VMT may be considered an environmental marker of vehicular traffic.
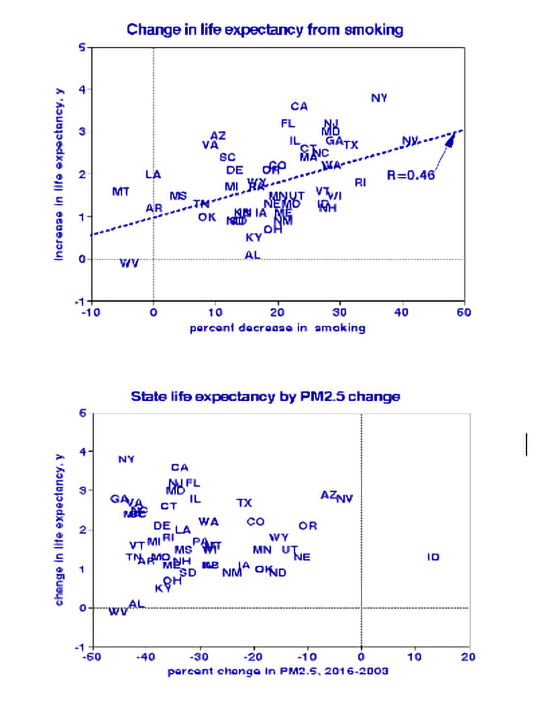
 As a check on these findings, I compared changes in state life expectancies from 2000 to 2019 with changes in smoking prevalence and mean PM2.5 concentrations, using state abbreviations as data points in the graphs. I found a strong relationship with smoking, indicating a life expectancy gain of about five years for 100% cessation, consistent with conventional wisdom. By contrast, I found no association between change in life expectancy and PM2.5 abatement; that was also the case with joint regression with PM2.5 and smoking and in stark contrast with current regulatory philosophy.
As a check on these findings, I compared changes in state life expectancies from 2000 to 2019 with changes in smoking prevalence and mean PM2.5 concentrations, using state abbreviations as data points in the graphs. I found a strong relationship with smoking, indicating a life expectancy gain of about five years for 100% cessation, consistent with conventional wisdom. By contrast, I found no association between change in life expectancy and PM2.5 abatement; that was also the case with joint regression with PM2.5 and smoking and in stark contrast with current regulatory philosophy.
- These are associations, not necessarily effects or causes.
- I assumed that state-level associations also apply to individuals.
- I did not consider the effects of external causes on all-cause mortality rates.
- I neglected changes in average demography over time (age, race, ethnicity).
- Life expectancy in the District of Columbia was an outlier and not included in some statistical analyses.
Conclusions
When using descriptive variables, this simple cross-sectional analysis found significant long-term associations with mortality similar to what others have reported: the beneficial effects of income and adverse effects of fine particle air pollution (PM2.5), vehicular traffic, and smoking. However, when I compared changes in putative causes and effects during the past two decades, only smoking and traffic were statistically significant, implying that increased income or reduced PM2.5 levels provided no significant benefits. This finding was reinforced by the finding that smoking cessation could lengthen life by about five years while reducing PM2.5 air pollution would have no such long-term benefits. This differential analysis offers the advantage of precluding the need for certain rarely available descriptive variables like indoor air quality and personal income.
If we’re interested in changing the future, we must begin by studying changes in the past.
Toward that end, it would be helpful to re-examine health effects stemming from air pollution accidents or interventions. I’m unaware of any epidemiology studies demonstrating longer lives due to cleaner air.
Sources
CDC Compressed Mortality Files, State-level Life expectancies, State-level Household income, State-level Miles traveled, and vehicular trips
Lung Cancer, Smoking, And Air Pollution – Vive La Difference!
The Tax Burden on Tobacco, 1970-2019 CDC
