It is seemingly such an easy question: if I need an ambulance, what will it cost me? Unfortunately, there's only a complex answer, summarized as “it depends.”
“It depends” begins with who is providing the ambulance, a government agency or private company, your health insurance or lack of same, your state, and whether you are in a rural or urban area. Additionally, ambulances can charge a fixed fee or have additional “add-ons” for providing advanced life support in the case of life-threatening emergencies or mileage.
Once you call 911, the ambulance closest to your location is dispatched. You have no control over whether that ambulance is provided by any of the three general types of ambulance services
- Government, including fire departments
- Community non-profit
- Private Non-Hospital
As a generalization, roughly 62% of ambulance transports are by governmental agencies (60% by fire departments), 22% by non-profits (about a third of that from health system ambulances), and 16% by for-profit services. Health system ambulances may be non or for-profit based on the status of their health system.
Ambulance charges – There’s a code for that.
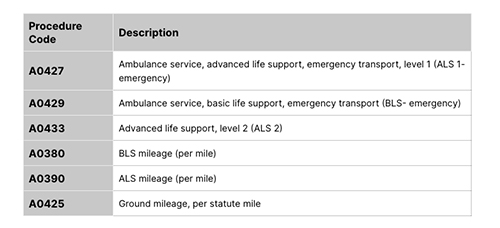
As with all billing in healthcare, there are codes indicating the service provided and the charges; charges vary based on where you, the ambulance, and the nearest emergency department are located.
 Basic life support is the care rendered by the ambulance crew of EMTs and paramedics that do not require “cardiac monitoring or respiratory interventions.”
Basic life support is the care rendered by the ambulance crew of EMTs and paramedics that do not require “cardiac monitoring or respiratory interventions.”
Advanced life support services provided by a paramedic (an EMT with more advanced training and privileges) are more invasive, managing airways, initiating cardiac support, etc.
As you can see, there are additional charges for these services based on the miles traveled by the ambulance. Local governments often set those rates. In New York City, the current charges are $20 per mile. In other instances, mileage charges are set by for-profit organizations. They can be much more significant and have been a source of “surprise billing” – ground ambulance transportation is not covered by recent federal “no surprise” legislation.
In general, an ambulance ride costs about $1300; when only basic life support is necessary, costs drop to an average of $950. As a study in Health Affairs reported,
“In this study, we found that commercially insured patients who underwent ambulance transportation received potential surprise bills in 71 percent of rides, and out-of-network charges exceeded in-network prices by $450 in ground transportation.”
Health Coverage – What are my costs?
As with all things in healthcare, it depends. Let’s take the simplest case first; you have no insurance or coverage. As you do with all healthcare services, you will be paying the full sticker price. You may be able to get a break for cash payments or set up a payment plan, but you are the individual “born every minute” that PT Barnum mentioned.
Medicare covers ambulance transportation to and between hospitals. Medicare pays 80% of what is considered a reasonable charge (e.g., that mileage payment is roughly $8/mile), and you pay the remaining 20%. Hospitals that do not participate in Medicare, and that is a tiny number, may charge 110% of Medicare’s allowable charges. Medicare will reimburse you 80%, so your overall out-of-pocket costs may increase slightly. That 10% difference is the only “surprise billing” a Medicare beneficiary faces. Medicaid covers emergency ambulance transportation provided by duly licensed ambulance services; non-emergent ambulance transport may be covered if the patient can provide physician documentation of need (a doctor’s note).
Private, commercial insurance coverage varies with the particular policy. As a generalization, all or a portion of ambulance costs will be covered for medically necessary transportation to the hospital. In some instances, what is medically necessary lies in the eye of the beholder, and what is an emergency to a patient may not be an emergency to their insurance company. Other variables are the deductibles, co-payments, and the most significant variable of all, whether the ambulance and the destination hospital are “in network.” This significant up-charge for services provided “out of network” is the greatest source of what has been termed surprise billing.
Surprise!
A surprise bill is just that, an exceedingly high charge for services you anticipated would be covered – they are due to the difference in charges of providers “in-network” and subject to billing limitations and providers “out-of-network,” where those limitations are more expansive and less enforceable. Given that when you call for an ambulance through 911, you have no choice of services, ambulance transportation costs are a big source of surprise billing.
The “No Surprises Act” prohibits balance billing, the term used for those increased costs to beneficiaries, for many out-of-network services, but not ambulance transportation. Ten states [1] have enacted regulations limiting these out-of-network charges for ambulance transportation but only apply to state-regulated policies – employer-funded plans are not covered.
The cost to the patient for ambulance transportation reflects the arcane systems we employ to cover our healthcare costs. Transparency in charges, the first step in reorganizing payment into a coherent, manageable system, remains aspirational rather than practical. The “No Surprises Act” had empaneled a workgroup to examine the chaotic payment system for ground ambulances. They began their work this May; a report is due in six months.
What’s a patient to do?
Many of the articles on ambulance costs offer some advice as to what to do. As a physician, this is a little too close to medical advice. It is so challenging to separate urgent from emergent, especially when those concerns involve your health. If you believe your life is at risk, call the ambulance and worry about the cost another day. At worst, if you are wrong, you will be stuck with a bill that you can haggle over – but if your life is at risk, then delaying care even for a short while can be deadly. The phrases “time is muscle,” used by cardiologists, and “time is brain,” used by neurologists, convey the urgency and efficacy of timely treatment for heart attacks and strokes, respectively.
[1] 
Sources: How Much Does an Ambulance Ride Cost? VeryWell Health
How Much Does an Ambulance Ride Cost Without Insurance?
How Much Does an Ambulance Ride Cost? GoodRx Health
Protecting Consumers from Surprise Ambulance Bills The Commonwealth Fund

