The concept of a “leaky” brain is an enigma, the fortress of our brain, seemingly protected by the blood-brain barrier now disrupted. However, to understand whether a breach has altered our cognitive function we need to better understand our protector.
“Leaky” Brain
Many patients with Long COVID complain of “brain fog,” a disturbing sense of impaired thought that is often but not consistently quantitatively measurable. A recent study in Nature Neuroscience used a form of dynamic MRI (termed DCE-MRI) to look at a group of individuals with and without Long COVID and with and without brain fog. DCE-MRI uses a blood-borne contrast agent to capture before and after images of the brain’s vasculature. It “possesses an unparalleled capacity to quantitatively measure not only perfusion but also other diverse microvascular parameters such as vessel permeability and fluid volume fractions.”
The researchers found that
“While standard diagnostic MRI scans showed no clinically relevant pathological findings in any participant … Stratifying the cohort into recovered, long COVID without brain fog and long COVID with brain fog [DCE-MRI ]revealed significantly increased [Brain Blood Barrier] permeability in the cohort with brain fog compared to recovered patients and patients with long COVID without brain fog.”
But to understand what that permeability may or may not mean, we must begin by understanding the brain’s special privilege.
Immune Privilege – Defender of the Brain
The brain, along with the eye, testes, and placenta, have barriers to protect them from the systemic effects of immune responses. These barriers include
- Physical barriers, like the blood-brain or blood-testis barrier, physically limit the entry of immune cells and molecules
- Secretion of immunosuppressive and immunotolerant molecules
- Lack of lymphatics reducing the presence of immune cells
The brain is among the most “immune-privileged” of organs primarily through the highly selective permeability of the blood-brain-barrier (BBB), its minimal lymphatic drainage, the presence of cytokines that “dampen” inflammatory responses, and microglia, the “resident” immune cell of the brain, that further reduce the effects of inflammation and immune cells.
However, immune privilege does not mean immune protected. The “leaky brain” hypothesis is predicated on presumed alterations of the BBB that allow the enhanced transport of immune cells and mediators that can wreck damage to the brain. While there is evidence that the BBB can be made transiently more porous or leaky, it remains scientifically unclear whether this is a cause or effect. We simply do not know.
The Gatekeeper, the Blood-brain-barrier (BBB)
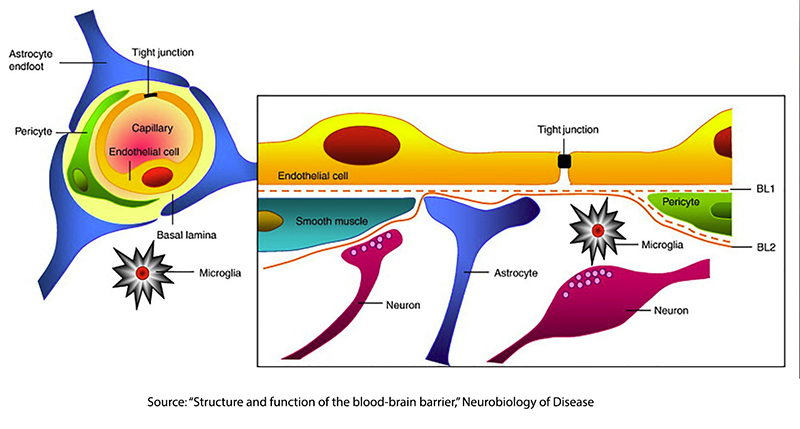 The BBB is highly specialized to meet the needs of our brain and dynamic in its changing structure. It consists of several cellular components:
The BBB is highly specialized to meet the needs of our brain and dynamic in its changing structure. It consists of several cellular components:
- Endothelial cells line the inside of our blood vessels, which are tightly connected, creating a physical barrier to the movement of cells and molecules from the bloodstream into the brain.
- A basement membrane provides structural support for the integrity of the blood vessel wall and, with its selective permeability, acts as a gatekeeper for access to the brain. It is a mistake to think of this membrane as some wholly solid structure. The molecular engines responsible for its selective permeability are free to move from one area to another, making for a shifting permeability
- Astrocytes are one of the brain's structural cells (glial cells) that surround the brain’s blood vessels and provide a cellular link between the neuronal circuitry and blood vessels to regulate the endothelial cells and tighten their junctions. Astrocytes are important mediators of BBB formation and function.
- Pericytes are contractile cell that helps control the diameter of the smaller blood vessels, the capillaries
Additionally, the BBB consists of various specialized transport systems. This includes glucose transporters that facilitate the entry of glucose into the brain, as it is the brain's primary energy source. Ion channels that regulate the inflow and outflow of sodium, potassium, and calcium play vital roles in the brain's electrical activity. And enzymatic protein transporters that can metabolize, detoxify, or serve as exit points for molecules entering the brain.
All of these components create a barrier between the blood and the brain that can be tightly controlled.
Breaching the Walls - Disrupting the BBB
Like all biological structures, the BBB's function is imperfect, and its role in creating “immune privilege” can be compromised. The physical barriers provided by the tight junctions may loosen in the presence of dysfunction of the astrocytes and pericytes, leading to fluid entering the brain. Inflammation acting through a variety of cytokines may attract immune cells that can further disrupt the barrier. As you might anticipate, oxidative stress can alter BBB permeability by denaturing some protein transportation systems.
These alterations can result in neuronal dysfunction by disrupting the ion balance, perturbing the transmission of electrical signals, and allowing the entry of harmful immune cells and molecules.
“Leaky” Brain Redux Navigating the Foggy Uncertainty
The concept of a disruption of the BBB resulting in increased permeability has its roots in a similar phenomenon seen in the gut in the presence of severe gastrointestinal infection. There is good evidence that in the presence of this form of sepsis, the gut’s tight junctions loosen and allow the enhanced bacteria transport into the bloodstream. But the gut is not an immune-privileged organ; it shares tight junctions with the BBB but has its own protective properties, specifically mucus, which is another physical barrier.
There is some evidence that clinical situations may result in significantly altered permeability of the BBB, creating a “leaky” brain. In a review of ischemic strokes and the BBB in Frontiers in Physiology, the researchers point to the disruption of blood flow and oxygen to the brain from these strokes that goes on to break down the protein transport systems and the mechanical coupling of the cells, those tight junctions, that leads to brain swelling.
There is also evidence that autoimmune diseases, including multiple sclerosis, can lead to a leaky gut due to both inflammation and dysbiosis, an alteration in the composition of the gut microbiome. This dysbiosis, in turn, has been found to lead to metabolites that “stimulate astrocytes to produce an MS-like disease in mice.” That said, BBB dysregulation is a feature of MS in humans.
“Multiple studies have shown BBB breakdown and dysregulated BBB transport in [Alzeheimer’s Disease] models, establishing their roles in neurodegeneration and development of Alzheimer’s Aβ and tau pathology.”
But a careful read of that sentence points to substantial scientific uncertainty. We do not know whether the “Aβ and tau pathology” is a cause or effect. Nor do we know whether the dysregulation of the BBB is a cause or effect.
The whisper of a correlation between BBB dysregulation and some neurodegenerative diseases has opened a doorway for the snake-oil salesmen, who mine the population distraught and hopeless in the face of their neurodegenerative diseases, offering them supplements that have little or no effect on the BBB, which in turn, may or may not be an underlying cause of their disease. Katie Suleta details the whispering of one of these grifters.
In the words of one reviewer,
“One short-coming of these studies for a leaky gut/leaky brain is that they fail to offer detailed explanations for the findings or a unifying construct, something more than anecdotal or post-mortem proof that a physiologic effect is unequivocal. I like to say that when it comes to opining on fringe concepts in medicine or complementary alternative theories in practice, ‘I like to keep an open mind. However, not so open a mind that my brains fall out’ or, in this case, leak out.”
The concept of a "leaky" brain presents a fascinating puzzle. As investigations continue to unravel the mysteries of the BBB and its role in conditions like Long COVID and neurodegenerative diseases, tantalizing correlations may spark curiosity, but it's essential to distinguish between evidence-based insights and speculative claims.

