The question of which diet is best for which people has led to some strange prescriptions, such as the worthless Blood Type Diet (see here for our take on this one). However, reputable researchers are looking for a means of telling who might do better on one type of diet rather than another. Thus Dr. Christopher D. Gardner from the Stanford University Medical School and colleagues investigated whether having information about a person's DNA makeup and/or their insulin secretion levels might inform the choice about what type of diet to choose. Their report was published in JAMA.
These researchers noted that while overall there's no big difference in the success of weight loss on low fat vs. low carb diets, there are indications that some people do better on one type than another. Thus, they hypothesized that knowing the genetic makeup with respect to 3 genes (PPARG, ADRB2, and FABP2) that are involved with fat and carbohydrate metabolism, and/or the levels of insulin secretion after glucose consumption, might indicate which diet would be more effective.
To test their hypothesis, they recruited 479 healthy, overweight or obese adults (BMI between 28 and 40), and aged 18-50 years. These people were randomly assigned to consume either a healthy low-fat diet (HLF) or a healthy low carb (HLC) diet for one year. Participants were instructed on which foods to minimize or maximize while on their particular diet. Their food intake was monitored by repeated 24-hour recalls, and physical activity was similarly self-reported. People with genotypes thought to be more sensitive to fat or to carbohydrates were noted. Initially, and at 6 and 12 months into the study participants were administered an oral glucose tolerance test*, and their patterns and amounts of insulin secreted in response to a 75-gram glucose challenge were determined — the 30-minute response was used as an indicator of carbohydrate sensitivity.
Initially, the groups didn't differ with respect to nutrient consumption. However, after participants were randomized at the 12-month time point, the HLF group's average consumption of fat was 29 percent of calories, while that of the HLC group was 46 percent. Carbohydrate consumption was 48 and 30 percent of calories for those groups, respectively. These data indicate that the groups were following their assigned protocols.
However, when the researchers tested for interactions among diet type and gene patterns at the 12-month point, there were no significant differences between the groups. Further, there was no effect of having a genotype and diet assignment that was matched or mismatched (i.e., having a low carb genotype and being assigned to the low carb vs. the low-fat diet). Similarly, there was no effect of level of insulin secretion at baseline and weight loss on either type of diet. And, as others have found, there was no significant difference in weight loss after a year on the assigned diets, as shown in the figure below.
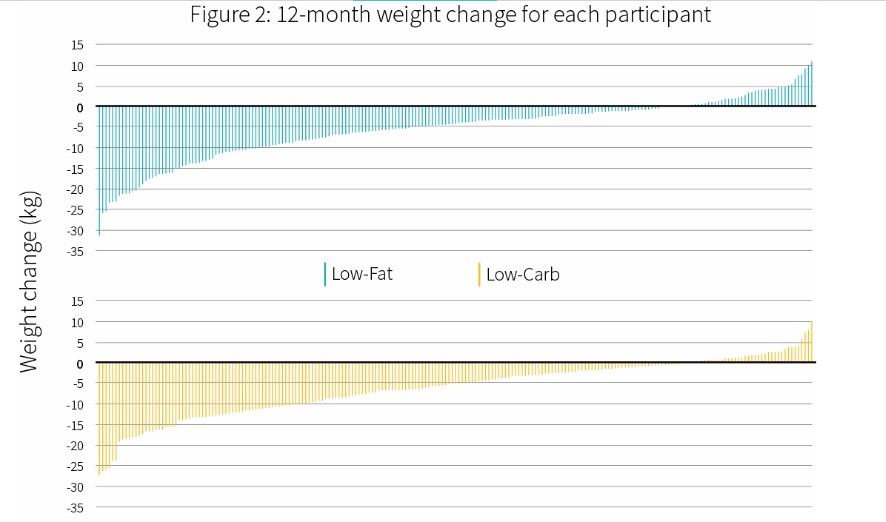 Figure courtesy of Examine.com
Figure courtesy of Examine.com
The researchers concluded:
"In the context of these 2 common weight loss diet approaches, neither of the 2 hypothesized predisposing factors [the genotypes or basal insulin secretion] was helpful in identifying which diet was better for whom."
Of course, this was a relatively small study that should be replicated. However, the obvious take-home message is that as long as a person chooses a healthy diet with which to lose weight, there's no reason to think that either low-fat or low-carb will automatically have a greater benefit. Further, it could still be possible that other factors, such as other genotypes, might have a predictive value for weight loss — that remains to be demonstrated.
*Oral glucose tolerance test is the measurement of blood levels of glucose and insulin at defined time points (e.g., 9, 30, 60, 90, and 120 minutes) after consuming a known amount (typically 75 grams) of glucose in a solution. The levels of each and patterns of secretion are used to pinpoint derangements in carbohydrate metabolism and diagnosis of diabetes.