As an avid reader of the New York Times, it pains me greatly to read about a familiar subject that has so many errors and misconceptions. Especially when COVID-19's impact on society is being discussed.
To begin with, the EPA rule in question is about ambient air quality standards, not emissions, even though the latter is responsible for the former. There’s a world of difference; we can measure emissions from tailpipes and smokestacks, but we know precious little about the ambient air that we all breathe, in large part because we live and work in environments that are not sampled.
Then there’s the definition of the pollutant in question, officially designated as PM2.5, also known as “fine” particles. It’s not a pollutant per se, being defined solely as particles smaller than 2.5 micrometers regardless of their chemistry or toxicity. PM2.5can be very different in the Lincoln Tunnel than in the Mohave desert or in your grandma’s kitchen. Particle size controls where it may deposit in our lungs, but its chemistry determines what subsequently happens.
This brings us to the question of soot, the appellation often used by the Times when they mean PM2.5. We all know soot, the black residue inside chimneys and tailpipes, but it’s only around 5% of airborne PM2.5, and its principal (60%) constituent tends to be non-toxic ammonium sulfate. Soot particles, denoted as elemental carbon (EC), are among the smallest and potentially toxic and can go where sulfate particles cannot, notably in the deepest regions of the lung and then into the bloodstream. Autopsied lungs from polluted cities tend to contain carbonaceous deposits, but the soluble sulfate particles are nowhere to be found. The problem in the attribution of health effects to PM2.5 is that the ambient air quality standards rarely measure the PM2.5 constituents most likely associated with the health effects cited in the article.
The new Harvard paper by Xiao Wu and colleagues “underscoring the importance of continuing to enforce existing air pollution regulations…” is not a bona fide scientific investigation because it considers only one pollutant and ignores others regulated under the Clean Air Act. It used aggregate information on entire counties, not actual air pollution exposures by COVID-19 victims, or their smoking, medical comorbidities, demographics, or socioeconomic status. It inferred those characteristics, thus committing the “ecological fallacy” (the whole cannot represent its parts). The long-term air pollution-mortality studies cited as support also suffers from this limitation; they lack information on personal exposures that are dominated by indoor sources such as passive smoking, cooking, cleaning, and pets. EPA has no mandate to regulate air quality indoors, where we typically spend 85% of our time and even more during hospitalization. Outdoor ambient air quality characterizes locations, not the personal exposures of inhabitants.
Recognizing this fundamental limitation, I undertook a confirmatory study of COVID-19 deaths at the state level, for which public data were readily available [1]. This paradigm has the advantage of studying mortality rates rather than death counts, thus removing a significant source of variation. It also allows us to consider and directly display the effects of other important risk factors such as race, smoking habits, household income, population density, all of which are attributes of places and avoid the ecological fallacy.
I considered five air pollutants: PM2.5, two of its constituents, elemental carbon [EC] and sulfates [SO4]), and two gaseous precursors (SO2 and NOx). EC and NOx have more local effects since they are mainly emitted by ground-level vehicular traffic; their concentrations peak in urban areas. SO2 is now mainly emitted by large industrial sources with high smokestacks. It oxidizes as it travels downwind to become SO4, the major constituent of PM2.5.
Potentially confounding variables included state percentages of smokers, racial percentages, median household income, and estimated urban population density. I used a simple regression analysis to determine relationships among these variables and graphs to display the most important. I used 2002-3 air quality data to allow for the known lag in developing chronic disease development. [2] This is what I found:
- Population density and each of the pollutants were significant predictors of COVID-19 mortality rates, individually.
- EC, NOx, and population density in combination with one or more other confounding variables remained significant, but PM2.5, SO2, or SO4 do not
I concluded that population density and traffic-related air pollutants were significantly related to COVID-19 mortality rates - parameters describing places but not necessarily individual exposures.
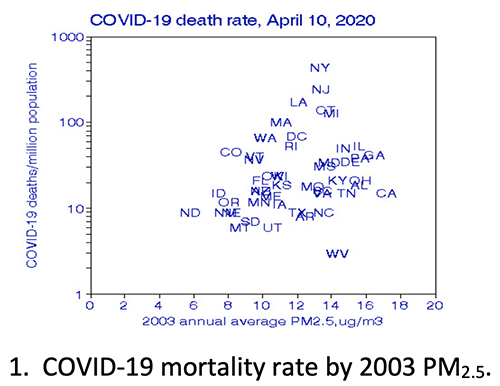 Figures 1 and 2 display these relationships; the state abbreviations represent data points. In Figure 2, COVID-19 mortality varies by about a factor of 10, from less than 10 to more than 100 deaths per million population. Wu reported that his statistical procedure predicted COVID-19 mortality would decrease by 15% if long-term PM2.5 were decreased by 1 µg/m3over 16 years – a percentage lost in the wide variation in COVID-19 mortality.
Figures 1 and 2 display these relationships; the state abbreviations represent data points. In Figure 2, COVID-19 mortality varies by about a factor of 10, from less than 10 to more than 100 deaths per million population. Wu reported that his statistical procedure predicted COVID-19 mortality would decrease by 15% if long-term PM2.5 were decreased by 1 µg/m3over 16 years – a percentage lost in the wide variation in COVID-19 mortality.
By contrast, my regression model predicts that decreasing PM2.5 by 10% would result in 4% greater mortality, but that 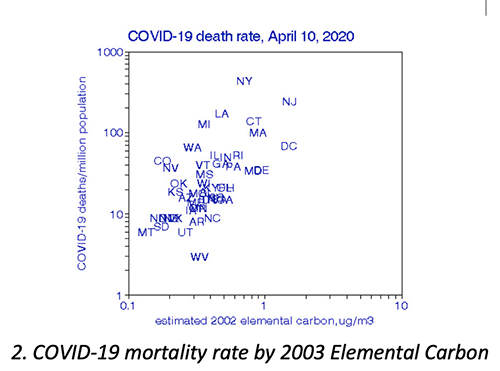 a previous 10% reduction in EC could cut COVID-19 mortality by 6.7%. None of these small increments are evident from the figures because of the large spread in the data.
a previous 10% reduction in EC could cut COVID-19 mortality by 6.7%. None of these small increments are evident from the figures because of the large spread in the data.
For comparison with the other mortality studies discussed in the Times article, I replicated this state-level analysis for 2016 circulatory disease mortality. I found smoking to be the most critical predictor with a mortality drop of 40% for cessation, while reducing PM2.5 was associated with a nonsignificant increase of about 0.7%. EC and NOx risks were about 7% and compared well with the all-cause mortality risks predicted in my previous analysis. [3]
There is another overarching problem with spatial studies like these in that people move as populations change. If a long-term California resident moved to New York and contracted COVID-19, Wu’s model would have assumed New York particulates were responsible.
Returning to the New York Times article, here’s what it got wrong.
- Misunderstood the pollutant in question.
- Failed to question Wu’s underlying analysis of COVID-19 mortality.
- Failed to distinguish between regulatory advocacy and scientific investigation.
- Neglected personal air pollution exposures of those most at risk, including COVID-19 patients.
- Failed to recognize that location does not imply causation.
[1] CDC Wonder Compressed Mortality Files
[2] Longitudinal relationships between lung cancer mortality rates, smoking, and ambient air quality: a comprehensive review and analysis. Crit Rev Toxicol. DOI: 10.1080/10408444.2019.1700210.
[3] Air pollution and survival within the Washington University-EPRI veterans cohort: risks based on modeled estimates of ambient levels of hazardous and criteria air pollutants. J Air Waste Manag Assoc. PMID: 19418821.
