As the possibility of an effective COVID-19 vaccine grows, there are questions of distribution. The first-come, first-served approach seems (and is) too random to save lives or the economy. We need some form of prioritization, and here we are in uncharted territory; there are no facts, only computer models. Let's consider one optimized to save the most lives.
COVID-19 is a global issue requiring a global solution. Vaccines, the essential component of our scientific understanding of herd immunity, is anticipated to be distributed to all the world's nations. Leaving aside how those global resources are equitably divided, and that is a big aside, how do we form the US's queue? Much of the back and forth over the Barrington Declaration and other options have to do with what you seek to optimize, lives, or the economy.
The Model
Of course, that is a false choice since the two are not independent, being heavily entangled. This study's model seeks to reduce fatalities and pressure on the pandemic's chokepoint, health system capacity. A limitation of the model is that individuals are stratified by age into groups. But within this broader classification, data is more specific for co-morbidities, interactions with other age groups, all the behavior, and factors that we believe impact being infected by COVID-19 and the subsequent outcome. [1]
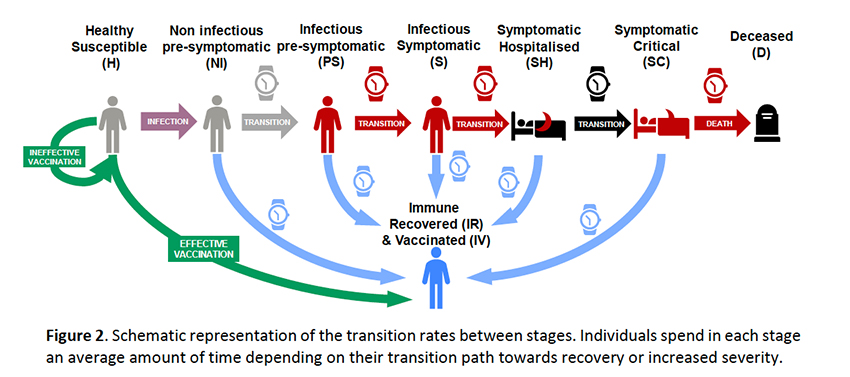
The simulation involves nine age groups [2] and uses the classic SEIR epidemiologic model depicted in this graphic based upon Spanish populations and data.
As with all models, the parameters can be manipulated, with the choice of parameters simplifying a real-world problem's complexity – you should look at the dynamic relationships, not the numbers. The model does not support varying densities, e.g., rural vs. urban. It assumes reinfection is not possible, that immunity is no different for those not vaccinated or ineffectively vaccinated, and that recovered individuals are equally eligible for vaccination as the healthy susceptibles. Most critically, immunization rates are proportional to the number of eligible individuals and are "limited by the capacity of their health system."
The Simulation
The outcome of the calculations is to minimize the deaths one month after the vaccination campaign is completed. At any given moment, priority is given to the group "with the highest number of avoidable deaths" – deaths that include group members along with the infections and subsequent deaths that would transmit to others; call it the Typhoid Mary component. Starting parameters include no pre-existing immunity and an initial 3-fold greater incidence of pre-symptomatic infections than symptomatic. Vaccination proceeds at a rate covering 1% of the population daily. Vaccination effectiveness was varied from 50% to 100%, and the population covered ranged from 50% to 95%. The numbers I am reporting on the two most likely initial scenarios of 50% efficacy and coverage. As I suggested, the relationships do not change, although the numeric outcomes do.
- The first-come, first-served, no priority vaccination was used as a baseline. It modeled 114,000 deaths or 0.24% of Spain’s population (equivalent to about 850,000 US lives lost despite vaccination)
- In every case, greater vaccine efficacy increased the covered population's size and reduced the total number of deaths. But whether the prioritization scheme this was an improvement or detriment remained unchanged.
- When priority was given based on those with the highest mortality per infection, and the group wholly treated before proceeding to other groups, deaths increased by 8.5% compared to the baseline first-come, first-served.
- When priority was given to those with the highest number of daily interactions, and its members completely treated before proceeding, deaths decreased by 21.6%
- As vaccination increases, those at-risk change. When priority was flexible to reflect day-to-day changes in the most significant projected mortality per infection, deaths decreased by 21.9%. This more dynamic protocol was only slightly better than when priority was given to those with the highest daily interactions.
- A dynamic computer model considering thousands of protocol variations, a practical impossibility, resulted in more lives saved, rising to 26%.
The Take-away
Ignore the numbers; consider their relative impact. First-come, first-served is not an acceptable public health policy. In addition to increasing the disparities in care already present in the system, it costs more lives. Counter-intuitively, vaccinating those at most significant risk of dying increases the lives lost, in part, because those at most significant risk often have less interaction with other groups – they are unlikely to be "superspreaders." While the greatest bang for the vaccine buck came from a highly optimized computer prioritization, it is impractical. Based on this simulation, our initial treatment should prioritize those with the highest number of daily interactions. The small gain from a daily tweaking of priority for those at the day's most significant risk is, again, logistically impractical. Imagine having to check whether you could go in for a vaccine every day after the computer calculation was performed.
From the point of view of lives saved, vaccinate those with the highest number of daily interactions. As a side benefit, in many instances, those are the people we need to re-open the economy. From a computational point of view, it may well be a win-win.
[1] The downside of this categorization is blending the spry apples from the frail oranges irrespective of age. As we make age more granular, the disparity of apples and oranges diminishes.
[2] "preschool children (ages 0-4); school children (ages 5-14); higher school and university young (ages 15-24), young workers (ages 25-49); mature workers (ages 50-59); senior workers (ages 60-64); early retired (ages 65-69); retired (ages 70-79); elderly (ages 80+).”
Source: Prioritisation of population groups with the most interactions for COVID-19 vaccination can substantially reduce total fatalities medRxiv DOI: 10.1101/2020.10.12.20211094

