Long COVID – the persistence of symptoms long past COVID’s normal recovery – remains in uncharted diagnostic waters. It’s a syndrome of symptoms rather than a specific disease. A new study from China sheds some light on who is at risk, and what symptoms they might have.
Let’s get the caveats out of the way. The data is from Chinese patients early in the pandemic, January to May 2020. China is not known to be forthcoming with data, and there is great suspicion regarding the numbers they do release. The dataset for this study is “not publicly available” but may be available “upon reasonable request and with the permission of the institution.” But as the saying goes, in the land of the blind, the one-eyed man, in this case, the current study, is king.
The study involved patients surviving their COVID hospitalization subsequently examined and interviewed 6, 12, and 24 months after discharge. Patients underwent a 6-minute walking test, laboratory work, and a subset underwent testing of their pulmonary function. Patients were stratified into three groups
- Scale 3 – no required supplemental oxygen
- Scale 4 – Supplemental oxygen
- Scale 5 – High-flow oxygen, non-invasive or invasive mechanical ventilation
Roughly half of the discharged patients completed the 2-year follow-up. Of those 1127, 230 underwent pulmonary testing. All were paired with control patients. Control patients were community-dwelling adults without COVID who were age, sex, and comorbidity [1] matched to COVID survivors.
The median length of stay was 14 days, increasing with the severity of illness. 36% of the Scale 5 patients were placed in the ICU (if US protocols were followed, that would suggest that 23% required mechanical ventilation as high-flow oxygen and non-invasive ventilation can often be provided in an area of heightened surveillance.) Patients received corticosteroids, antivirals (hydroxychloroquine and chloroquine were used in less than 1% of cases), immunoglobulins, antibiotics, and thymosin (an agent felt to stimulate T cell development). Again, these agents were used more frequently in those that were more severely ill.
 The first table demonstrates the symptoms present a 2-year follow-up; sleep difficulties, fatigue, and muscle weakness predominate. The percentages had diminished over time. The mMRC score is a measure of dyspnea, the perceived difficulty in breathing (>1), that too had diminished over time and oddly was less than that experienced by the community-dwelling controls – could China’s air quality be playing a role? The EQ-5D-5L questionnaire measures quality of life, once again improving over time, but there clearly are differences between those considered to have “Long COVID” and the controls. This is most marked in pain/discomfort and anxiety/depression.
The first table demonstrates the symptoms present a 2-year follow-up; sleep difficulties, fatigue, and muscle weakness predominate. The percentages had diminished over time. The mMRC score is a measure of dyspnea, the perceived difficulty in breathing (>1), that too had diminished over time and oddly was less than that experienced by the community-dwelling controls – could China’s air quality be playing a role? The EQ-5D-5L questionnaire measures quality of life, once again improving over time, but there clearly are differences between those considered to have “Long COVID” and the controls. This is most marked in pain/discomfort and anxiety/depression.
Physical findings also demonstrated some differences. Patients felt to have Long COVID walked about 12 meters over six minutes than controls [2]. Pulmonary function showed some losses in capacity and oxygen diffusion in each group, but it was markedly impaired in those patients requiring high-flow oxygen or mechanical support.
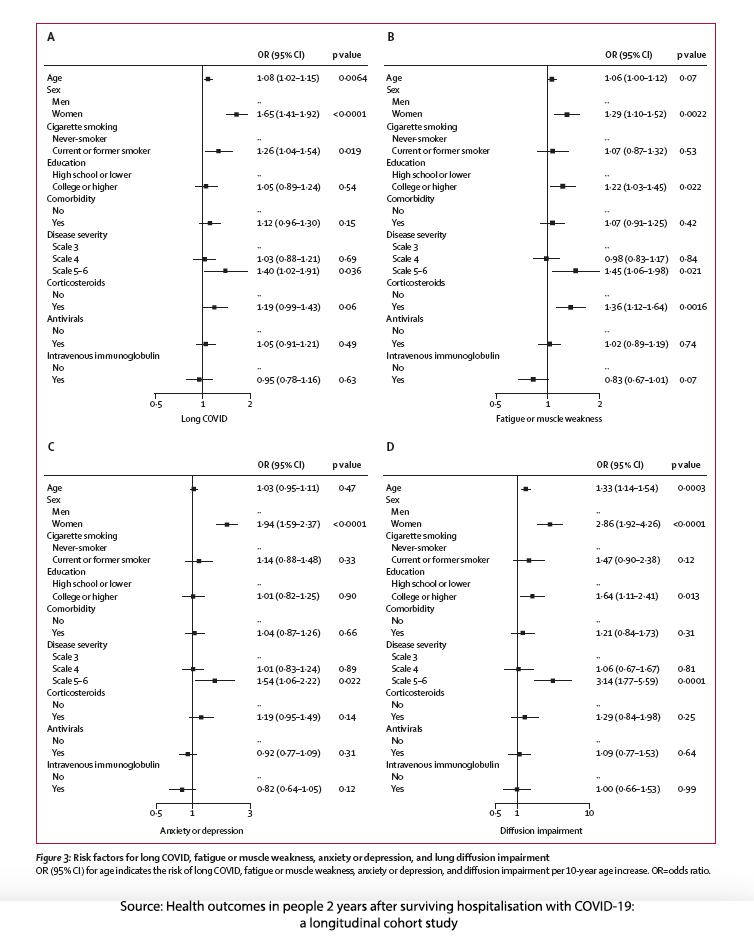
The study also provides our old friend, the Forest plot. As a gentle reminder, those horizontal lines touching the vertical are, by definition, not statistically significant.
Two risk factors stand out, being a woman, and being severely ill. Why might that be?
Could hormonal cyclicity play a role? The current thinking is that estrogen presence may be protective. The average age of menopause in China is roughly 48, 9 years younger than the median age of the patients. Additionally, women generally are more forthcoming about their health issues. Numerous studies, such as this one from Canada, suggest women speak up while men continue to believe that “real men” don’t cry or complain.
The severity of illness definitely plays a role. The more severe the condition, the greater the physiologic and metabolic hole you dig; climbing from that hole to recovery takes longer. For those that are very fit, digging out is not as great a project as it is for the less fit, let alone the frail. In many instances, those just shy of frailty, after a severe illness, found that they can no longer function on their own and require assisted care, temporarily or permanently.
Long COVID remains enigmatic. This study has suggested that those who were most ill continue to experience symptoms – that recovery is more complicated. There is a hint that gender may play a role and frailty most certainly does; we have yet to understand how those two “risks” interact with COVID recovery. In the meantime, we have increasing evidence that some experiences of COVID leave some with mental and physical hurdles. The best way to prevent Long COVID is, of course, not to become ill, or in our age of antivirals, consider their use early in your treatment course.
[1] Comorbidities include “cardiovascular disease, chronic respiratory disease, chronic kidney disease, hypertension, and diabetes.”
[2] At an average walking speed for the median age of this cohort, controls should have been able to cover roughly 514 meters, meaning the deficit among Long COVID patients of 12 meters was about 2%.
Source: Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study The Lancet DOI: 10.1016/S2213-2600(22)00126-6