For those who are too young to remember the early 1980s, the recent BBC News report, "HIV life expectancy 'near normal' thanks to new drugs" may not seem earth shattering. But, for those of us who do remember, what is reported in the summary of a new study published in the journal The Lancet, is nothing short of miraculous.
A 20-year-old HIV+ man who took antiretroviral therapy after 2008, living to be 78 year - not very different from the rest of us? Impossible. And now one-third of HIV+ patients are now over 50? Unimaginable. In the early days of AIDS, if you were infected with HIV when you were 20, maybe you'd live to see 25, but probably not. And those five years would not be pleasant.
Nothing can illustrate the stark differences between 1982 and today better than Randy Shilts’ iconic book, "And the Band Played On," which depicts the terrifying carnage inflicted by HIV during the early days of AIDS. Shilts, who was a journalist for the San Francisco Chronicle was one of the loudest voices during those dark times. He succumbed to the infection in 1994 – one year before the tide began to turn. It is truly unfortunate that he could not live a year longer, since he would be able to hear how quite band is now.
If you do remember the early days of AIDS, as do my friends and I, life could not be more different now than it was then. The results from The Lancet would have been considered science fiction or fantasy only three decades ago.
My friends and I sure remember, because it turned out that we were right in the middle of it. In 1982 a bunch of us were sitting on the deck of one of our parents' homes on Fire Island, when someone opened the May 31,1982 issue of New York Magazine. Inside was the first article to appear in the popular press about a nightmarish new disease that was killing gay people in ghoulish ways. None of us had seen anything like it, nor did we have even a reasonable guess about what caused it. One other fact that we certainly didn't know was, at that exact time, we were only four miles down the beach from the epicenter of the east coast AIDS epidemic. (1)
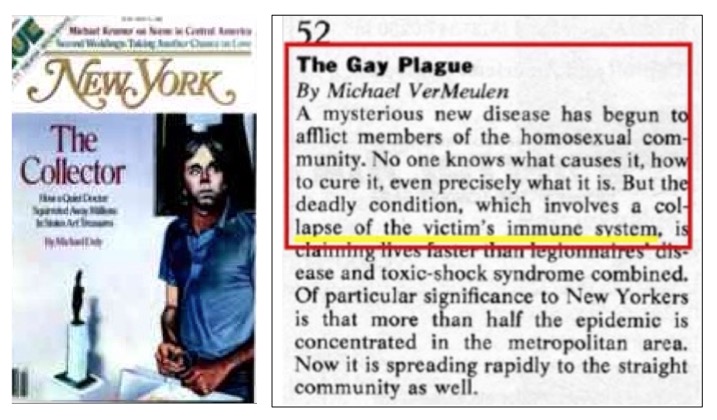
New York Magazine, May 31, 1982. Cover (left) and the beginning of the article (right). Terrifying.
Fire Island consists of 17 eclectic communities, two of them almost entirely gay. In one of these communities, Fire Island Pines, an Air Canada flight attendant named Gaetan Dugas, had been sharing a beach house with three other men. Dugas would later become known (incorrectly) as "Patient Zero"—the man who started the epidemic (Figure 1). Before long, everyone in the house would be dead, and in subsequent years, so would be most others in The Pines and its neighboring community, Cherry Grove. At that time, the disease, later called AIDS, had no name (2), nor did anyone know its cause. While many of these questions would be answered within a year, it would be yet another 12 years before help would arrive. (3) We were unknowingly watching the beginning of a worldwide epidemic of one of the scariest infectious disease ever known; one with a 100 percent mortality rate.
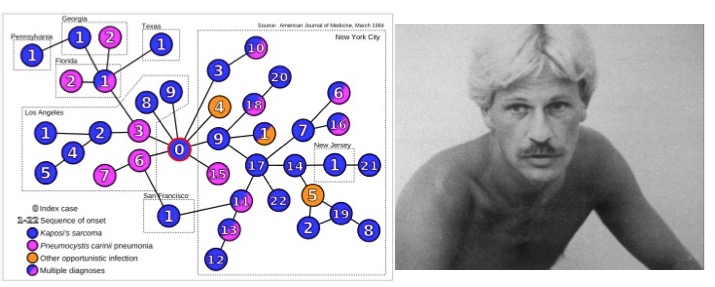
Figure 1. The first epidemiological study that identified Gaetan Dugas as Patient Zero. This would later be disproved. The nickname was coined as a time-saving abbreviation by NIH scientists, not for the public. The term stuck anyhow.
Source: The American Journal of Medicine
The battle to find a drug to control the infection was slow, frustrating, and brutal. There was one false hope in 1987, after AZT (Zidovudine) was approved by the FDA. But the drug failed dismally. AZT neither controlled the infection nor extended the lives of patients. The time between AZT's failure and the mid-1990s were the darkest days of the epidemic; one failed experimental therapy after another, after another, with little hope in sight. Hospital wards were brimming with dying men, but there was nothing that could be done for them.
It wasn't until late 1995—14 years after the first report of the virus first appeared in MMWR (4) —that Roche's saquinavir (brand name Invirase), the drug that made the first AIDS cocktails possible, was approved (3). Invirase, which was the first member of a class of drugs called protease inhibitors (PIs), works by inhibiting HIV protease, one of the essential viral enzymes required for replication of the virus. The results were dramatic. For the first time ever, the number of AIDS deaths in the US fell (Figure 2). In 2011, medicinal chemistry blogger Derek Lowe asked his readers "What’s the Most Worthwhile New Drug Since 1990?" Although there were a variety of answers, Saquinavir was often cited.
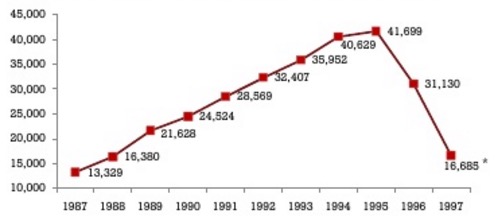
AIDS deaths in the US by year. Source: National Center for Health Statistics
By the late 1990s things really began to take off (4). Following saquinivir, different drugs were developed, which worked by other mechanisms—always desirable in the battle against pathogens. With more options came more possible combinations, and patient outcomes continued to improve. A total of 10 Protease Inhibitors were approved between 1995 and 2005. Although these drugs were critical at the time, PIs are rarely used today. Not only are better drugs available, but the PIs carried with them serious side effects, such as, nausea and vomiting, stomach pain, headaches, lipodystrophy (Figure 3), liver toxicity, diabetes, and skin rashes. Furthermore, PIs are not well absorbed in the gut, so large doses were required. This resulted in a high pill burden (Figure 3) on patients, and required that they take as many as 30-40 pills every day at regular intervals on an empty stomach. This meant that patients had to get up in the middle of the night to take a handful of pills. During the time that PIs were being phased out; "PI-sparing regimens" became a preferred cocktail.
(For a discussion of how PIs work see: ("The Water Molecule That Killed 34 Million People").
(Left) An example of lipodystrophy caused by protease inhibitors. Source: The Daily Kos
(Right) Daily pill burden, then and now. Source: Gilead Biosciences
By the late 1990s, almost every company in the pharmaceutical industry, including mine, had an ongoing HIV program, and the drugs continued to improve. In all, total of 35 (5) drugs belonging to six different classes (6) have now been approved in the US, and these have formed a very powerful arsenal against this once-deadly infection.
An ironic measure of how well the drugs work is an unintended consequence: When HIV meant a death sentence; people were so terrified that condom use was standard. But now, HIV is typically regarded as just another infection that just requires one pill per day to prevent AIDS. No big deal. As a result, unprotected sex in gay men is now commonplace, so much so that there has been a substantial increase in the incidence of other sexually transmitted diseases, for example, syphilis:
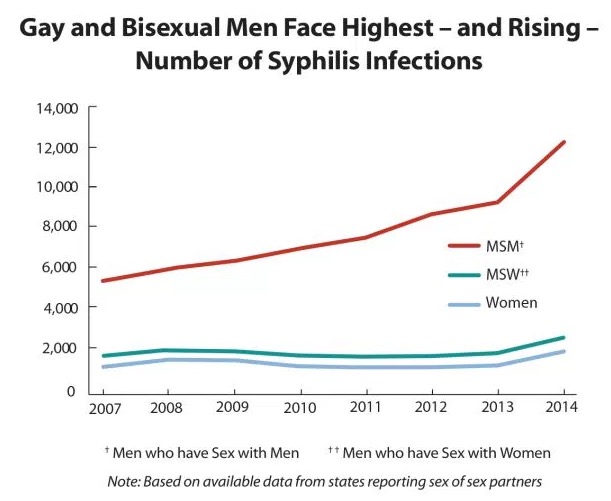
The number of syphilis cases in men who have sex with men more than doubled between 2007-2014. Source: CDC
The AIDS drugs are now so good that they can be used to protect seronegative people from infection by their seropositive partners, either before (pre-exposure prophylaxis ,PrEP), or after (post-exposure prophylaxis, PEP) unprotected sexual intercourse. The drugs also prevent transmission of the virus from infected mothers to their fetuses, and this marked the onset a worldwide effort to prevent the spread of the infection to children. In 2015, the World Health Organization recognized Cuba as the first country to stop all mother-to-child transmission. Later, Thailand, Armenia, Belarus, and the Republic of Moldova would follow.
So, AIDS has been brought under control in a manner that no one could have ever envisioned by making use of expertise in chemistry and biology, unprecedented manpower, and perseverance. One question that is rarely discussed is who deserves credit for this historic accomplishment - government, academia, or industry? The answer is all three, but in different ways (See Table 1 below).
Much of the knowledge of the fundamental biology— essential in unraveling the inner workings of HIV before drugs could be designed to attack the weak points of virus— came from academic and government research, but almost of the drugs that helped win this battle came from the industry. So, for almost all of the AIDS drugs, the scientists for drug companies were named as inventors (7), so they get the credit for that drug. This should not be taken as a slight to academia and government research, because no institution other than the pharmaceutical industry can match the knowhow, resources, and infrastructure that are required to do one of the hardest jobs in the world—discover a new drug. (8) But none of this would have occurred without a deep understanding of the science behind it. There is plenty of credit to go around.
Here's what tamed AIDS: Multidisciplinary teams in both the public and private sectors, made up of very sharp, dedicated, and tenacious scientists performing different but complimentary tasks. And, what a job they all did.
. Notes:
(1) Greenwich Village is also called the epicenter of the east. The distinction is largely irrelevant. Many gay Greenwich Village residents go to Fire Island on weekends.
(2) In September 1982 the CDC decided on the name Acquired Immunodeficiency Deficiency Syndrome.
(3) By 1983, much more was known about the virus: transmission from men to women, infection due to injection of drugs, hemophiliacs caught it from transfusions, Haitians were disproportionately affected. The CDC released its first official report on risk factors, much more...
(4) MMWR is the abbreviation for Morbidity and Mortality Weekly Report. It is issued every week by the CDC.
(5) There are 35 approved drugs, but 11 of them are mixtures of different drugs in one pill or reformulated versions of the same drug. I have omitted all of these. There are 24 unique chemical entities.
(6) Although Saquinivir was the first protease inhibitor, it was the sixth antiviral drug approved. All other drugs at this time were members of a single class called Nucleoside Reverse Transcriptase Inhibitors (13 in total). Some are still used today. Saquinivir is not. Cocktails work better when they are composed of different classes of inhibitors.
(7) An invention is defined by the names on the patent. This is part of the Constitution. All patents of drugs that came from industry will contain the names of the actual scientists. We then assign the patent to the company, and earn no revenue from the product.
(8) The title of this article is taken from the iconic book, "And the Band Played On," which depicted the carnage during the early days of AIDS. It is both fascinating and horrifying. The author, Randy Shilts, a journalist for the San Francisco Chronicle, was one of the loudest voices during those dark times. Shilts succumbed to the infection in 1994 - one year before Invirase was approved.
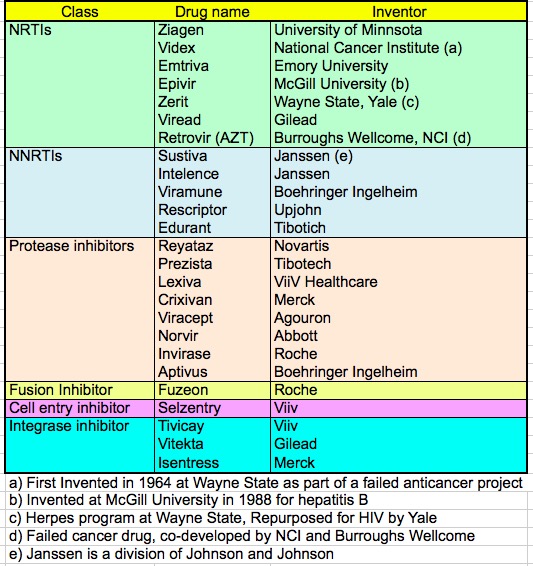
Table 1.The inventors of AIDS drugs. Of the 25 approved drugs, some came from academia, one from the NIH, and the rest from industry. This is another example of the complementary roles of academia and industry in drug discovery and development.