As if having cancer were not enough to worry about, people undergoing chemotherapy need to keep bacterial infections in the forefront of their concerns at all times. Now, a group from Flinders University in Australia presents a model that suggests that chemotherapy may make bacterial infections worse.
A new opinion article in Trends in Microbiology entitled, "Not Just Antibiotics: Is Cancer Chemotherapy Driving Antimicrobial Resistance?, presents a theory that chemotherapy creates a perfect storm within a cancer patient's intestine that creates antibiotic resistant bacteria, allows them to multiply and leak into the bloodstream through a damaged gut lining, resulting in antibiotic resistant bacteria in the blood - an incredibly dangerous and potentially deadly situation.
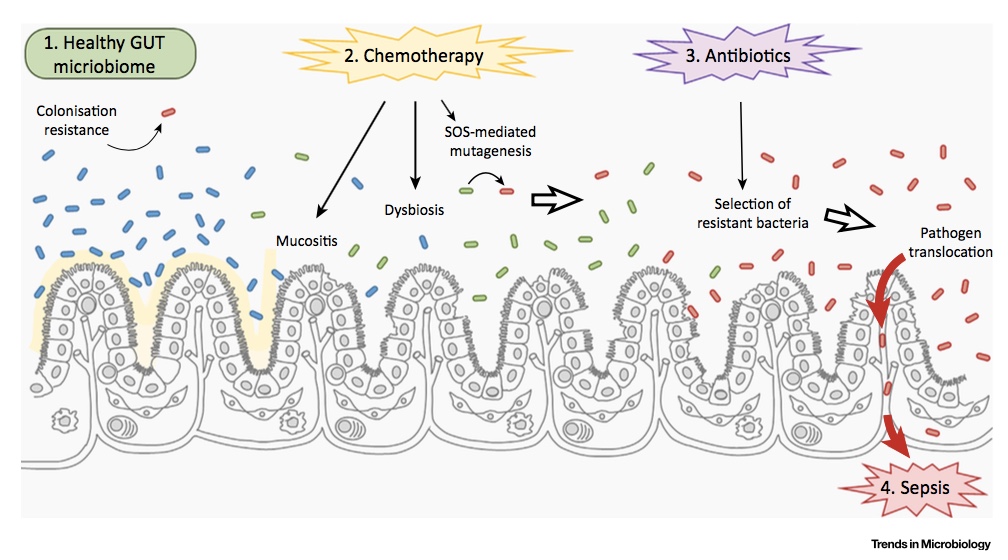
The model starts with a healthy intestine where there are a ton of bacteria present (the microbiome), playing many important roles to maintain gut health (see the left side of the figure below). These bacteria are termed "commensal" and, as long as they stay in the intestine, will do no harm. In fact, to take it one step further, they are important to keep the otherwise harmful bacteria (pathogenic bacteria) from colonizing the intestine.
The problem comes when the system gets perturbed, which is exactly what chemotherapy does in multiple different ways.
First, chemotherapy damages the intestinal wall, called mucositis (see the middle of the figure below,) leading to inflammation and loss of cells of the lining of the gut. When this happens, the normal barrier that keeps the bacteria contained is broken down increasing the chance that bacteria slip through and enter the bloodstream.
Chemotherapy is not only toxic to the cells of our body (which is why it is so effective as a cancer treatment) but it is also toxic to bacteria. In turn, it activates a response in bacteria called the SOS response which has two different outcomes. The first is an increase in the number of mutations in DNA which means more bacterial mutants. These new mutants could also be strains of bacteria that are antibiotic resistant.
On top of the increasing antibiotic resistant bacteria, chemotherapy can also cause the bacteria to exchange that resistance and share it amongst each other, resulting in a population of bacteria that is entirely antibiotic resistant (see the right side of the figure below).
So, in a cruel twist of fate, chemotherapy not only destroys the lining of the intestine but increases the number of antibiotic resistant bacteria at the same time. Unfortunately, there are currently few options available to break up this cycle. The first consideration would be to restore normal gut flora. This is certainly an effective approach in treating Clostridium dificile infections where normal fecal flora are transplanted into patients. Of course, probiotic supplements are also under consideration, but to date there is no specific therapy for protecting patients receiving chemotherapy. It is becoming clearer with time that our bodies are networks of interactions, and that perturbing one system has ramification in others. Understanding the way that these systems interact will allow us to better define ways to fix our unintended consequences.