Those with liver failure face at least two significant obstacles even before they can hope to receive a healthy replacement organ.
First, available livers in the United States are in short supply. Second, many of the ones that do become available for transplant often must be discarded, due to deterioration that occurs during the few hours the liver can remain healthy and viable while being transported from donor to recipient.
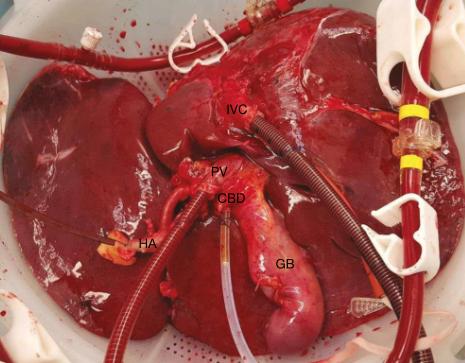
But a new machine being tested has the potential to lessen the impact of these formidable issues. The big change is that instead of livers being transported packed in ice, they are sent at normal 98.6o F body temperature in a warm bath of nutrient-infused liquid. And in this small study, that difference has produced encouraging results.
Using this method, which includes attaching the liver to a machine that pumps blood through the organ, European researchers found that there were 50 percent fewer livers discarded, resulting in 20 percent more of the organs being transplanted in those in need. Further, one year after transplantation nearly 66 percent of harvested livers using the warm-bath method – known as normothermic machine perfusion, or NMP – were functioning, as compared to 58 percent that were transported via ice-packed, static cold storage, or SCS.
 In its findings, published in the journal Nature, the research group known as the Consortium for Organ Preservation in Europe wrote that "[to] our knowledge, this is the first randomized controlled trial to compare any type of machine perfusion technology with conventional static cold storage in human liver transplantation."
In its findings, published in the journal Nature, the research group known as the Consortium for Organ Preservation in Europe wrote that "[to] our knowledge, this is the first randomized controlled trial to compare any type of machine perfusion technology with conventional static cold storage in human liver transplantation."
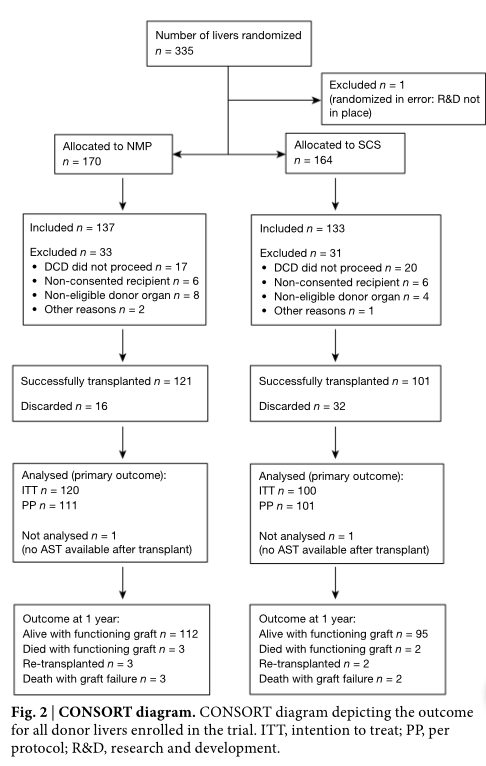
To start, the study involved 334 livers, of which 170 were shipped to hospitals in Spain, Belgium, Germany and Great Britan using the warm-bath version, while 164 were transported to those same countries in chilled, conventional fashion. After 64 livers were excluded for various reasons, 121 NMP-delivered organs were successfully transplanted versus 101 shipped by SCS.
In the process, only 16 NMP livers had to be discarded, as compared to 32 shipped on ice that doctors concluded were no longer viable – a reduction of 50 percent. Meanwhile, of the 170 NMP livers transported, 112 (or 66%) were functional a year after surgery, while 95 of 164 (58%) livers transported packed in ice were working.
"There were over 50% fewer discarded organs in the NMP group, resulting in 20% more transplanted livers," the study's authors wrote, adding speculatively that an "increase of 20% or more in the number of transplantable donor livers would have a transformative effect on the mortality on liver transplant waiting lists around the world."
There were a few reasons for the improved success rate. Primarily, because the warmed livers received oxygenated blood and continued to produce bile – an important indicator of functionality – they remained viable for transplantation for up to 12 to 13 hours before showing signs of deterioration, and up to 24 hours in all. That's a significant improvement over SCS-shipped livers, which are usually flushed with preservation fluid and can only remain viable for 7 to 8 hours and 12 hours maximum.
In addition, this extended viability allows for organs to be sent longer distances, allowing doctors greater flexibility to match the liver with the best recipient, which, in turn, increases the chances of a successful and long-lasting transplant. Another advantage of the new method is that upon receiving the warmed liver, surgeons can physically see how the functioning organ looks, and how it's working. That helps eliminate some guesswork regarding whether the cold-packed liver will eventually function properly, since it arrives in the operating room cold and gray and must be warmed before its positive attributes can be seen.
Today, there are 14,000 candidates for a liver transplant on the nation's waiting list, according to the United Network for Organ Sharing, an organization that governs transplants all organ transplants in the U.S. In 2016, roughly 7,500 liver transplants were performed.
Clearly, the new machine, called the "metra" and manufactured by OrganOx, is a much more expensive option than the conventional, ice-packed method of organ delivery. Metra is being used experimentally in the U.S. But if it eventually receives approval from regulators, many more transplant candidates may find themselves getting a potentially life-saving call.
"As well as demonstrating improved graft preservation," researchers wrote in their paper, "this trial tested the feasibility, usability and safety of NMP, a vital component of the evaluation of any new technology. It showed that the logistical challenges of NMP can be met successfully within clinical practice."