Humira, Enbrel, you see their ads regularly; they are part of a class of medications called biologics. Biologics provide relief for about 2% of America’s population at the cost of about 40% of the money we spend on pharmaceuticals. They are very expensive, rivaling the drugs used to treat cancer. The physicians who prescribed these drugs, predominantly rheumatologists released a position paper on biologics “generic” substitute, biosimilars. What are they saying?
Biologics and Biosimilars
Most of the medicines we use are not biologics but simple compounds created in Big Pharma’s factories. For these drugs, a generic equivalent is identical to the branded drug it is copying. To fast track generics, the FDA requires a single test demonstrating that the generic’s ability to be absorbed, excreted and utilized, it pharmacokinetics, is identical to the brand product and then allows its use for the same indications as for the brand product.
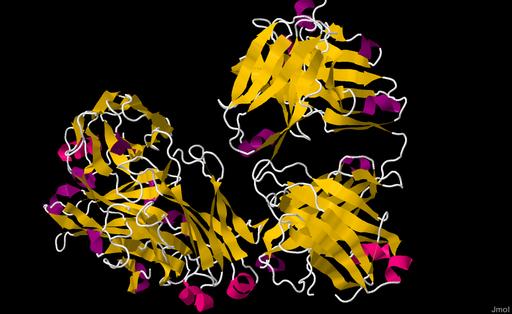
Biologics are complex molecules, modifying our immune responses to specific chronic inflammatory conditions like rheumatoid arthritis, psoriatic arthritis, or irritable bowel disease. They are manufactured by placing genes into host cells who through transcription and translation provide the core protein. Biosimilars are biologics “generic” equivalents, except they are not.
The reverse engineering of the DNA, choice of a host cell and the subsequent isolation and purification of the core protein make them similar but not identical. In the lock and key world of drugs, where a drug, the key, must fit into another structure, the lock, to be effective, the shape of that key may mean the lock opens, or doesn’t, or even require a bit of twisting and finagling. Biosimilars have an identical primary structure as their biologic but other factors, influencing shape may and do differ.
How the FDA approves these slightly different keys and their impact on the care of our patients, that is the first concern of the rheumatologists; the second is the cost and economics.
The impact on patients
The FDA requires a series of tests to term a new agent biosimilar. It must have an identical basic structure as the biologic, although it may have those other differences that alter its shape and possible efficacy. It must be proven to have the same pharmacokinetics. The body forms antibodies to these drugs; they are after all biologic compounds. Antibodies to the drugs may reduce its effectiveness, requiring higher dosages or more frequent dosings. A biosimilar’s immunogenicity can be no greater than its biologic equivalent. Finally, the drug must be shown in a study to be clinically equivalent to the biologic for one of the diseases it will be treating. It is the fact that it is tested on only one indication but is subsequently approved for other non tested indications that generates the controversy.
Extrapolation of indication
Trials are expensive and clinical trials for every indication drive up costs quite a bit. The FDA and its European counterpart facilitate speedier approval by saying, in essence, that if a biosimilar works for one indication and it is clinically equivalent to the biologic, then we can infer that it will work for all the indications. That logic stands on firm ground when drugs are identical, but biosimilars are not, they are similar. For example, some biosimilars have gained approval for pediatric indications, by extrapolation from studies on the biologic, they have never been clinically tested on children. As the white paper states, “Extrapolation continues to be an area of uneasiness among clinicians who are surprised to find that a biosimilar may be approved for an indication, … in the absence of clinical trials conduction in those patient populations.” Physicians are accountable for their prescriptions of therapy. But physician accountability is not matched by physician control.
Non-medical substitution
In the course of care, a physician may determine that one drug is less effective or has more adverse side effects and will change their prescription. Substitution, on the other hand, is when someone other than a physician substitutes one drug for another. These changes, often by a pharmacist, are regulated by state law. Non-medical substitutions are made more frequently, on a medically stable patient for reasons other than the drug’s efficacy or side effects – they are cost decisions. Decisions made by payers based on their tradeoff of efficacy and cost.
State laws vary as to how much influence the prescribing physician over these non-medical substitutions, and when they are notified. As you might expect, for physicians who remain accountable, this loss of prescriptive autonomy is of concern. More importantly, who knows the patient best, physician or insurance company?
Following the money
The primary reason to substitute a biosimilar for a better-investigated biologic is cost. From an economic point of view, competitive biosimilars should reduce the cost of both the branded and the generics; as it has with generics. But producing biosimilars is expensive, making it a challenging market for new competitors to enter. Given the difficulties in obtaining biosimilar approval in terms of time and cost, the marketplace is not going to have the multiple biosimilars required to promote price competition. The first biosimilar was discounted 15% from its biologic equivalent, so greater savings are unlikely at this point.
The opacity of drug pricing raises additional concerns of the rheumatologists described in the position paper. Insurance companies and their pharmacy benefits managers earn income based upon a percentage of the drug’s cost; costs we have no real way to determine. Irrespective of the actual price, income’s is predicated upon a percentage of the average wholesale price, so there is no incentive to lower prices. A biologic has a greater wholesale average price than a biosimilar; but a clever combination of discounts and rebates will reduce the biologic’s real price to a level competitive with a biosimilar - why purchase the biosimilar? For the pharmacy benefits manager, who help create discounts and rebates but are paid based on the higher wholesale average price, it means more income keeping biosimilars off their formulary. The position paper believes that current and future regulation will correct this problem.
The editorial that accompanies the paper is more direct essentially calling it a rigged game. Pharmacy benefits managers are often owned and operated by pharmacies and insurance companies. [1] Biosimilars can reduce costs, but for whom? A patient’s out of pocket expenses for biologics and biosimilars are almost identical, so patients are not saving money and consequently access to these forms of therapy remains limited.
Physicians also have a dog in the cost of care race. These medications are often infused, and there is an administration fee paid for the person infusing the medication. Typically it is a percentage of the drug’s cost, a flawed methodology since the cost of the equipment and time for administration of drugs has no rational reason for varying with their expense. A $10,000 drug that infuses over an hour requires no greater administrative costs than a drug costing $1,000, yet the administrative payment is ten fold greater. Ophthalmologists, prescribing the biologic Lucentis, in place of a far less expensive alternative and pocketing the greater administration payment demonstrate the problem.
Physicians have raised two concerns. First are these drugs clinically equivalent? Second, will the market forces we have seen in generics be the same as for biologics – will there be sufficient competition to significantly lower cost and improve access? These are identical concerns raised by oncologists who prescribed similar high-cost drug therapies. Should we begin to listen to these physicians, the ones providing us care? Are these rising concerns, random chirping or are they the canaries in the coal mine?
[1] This is a concern in considering the anticipated merger of CVS and Aetna.
Source: The Science Behind Biosimilars Arthritis and Rheumatology DOI 10.1002/art.40388
Source: The American College of Rheumatology White Paper on Biosimilars: It Isn't All White—There Is Some Gray and Black DOI 10.1002/art.40402