In addition to the numerous metabolic problems (e.g. diabetes) associated with obesity, we can add problems with lung function. For example sleep apnea, a condition in which a person repeatedly awakens from sleep because of breathing problems is significantly associated with obesity. Other than this type of problem, which seems to be associated with mechanical restrictions, researchers question whether obesity, particularly abdominal obesity, is related to decreased lung functioning and whether such decreases are reversible if a person becomes less obese. Further, if excess fat around the middle is the issue, does it matter if that fat is subcutaneous (just under the skin) or visceral (around the abdominal organs).
A group of researchers led by Dr. Eun Kyung Choe from Seoul National University Hospital Healthcare System Gangnam Center, Seoul, South Korea, studied the association between abdominal obesity and lung function — their study published in PLOS One. These investigators used clinical records from about 1100 adult Korean people — 428 men — assessing them at baseline and following them for about 3 years. All were healthy at the beginning of the study, and all were non-smokers who had never smoked.
As part of general health exams, these individuals had computed tomography (CT scans) which allowed the researchers to directly measure their body fat, and in particular to assess the amount of abdominal fat that was subcutaneous or visceral. In addition to several metabolic parameters, the researchers also had information on 2 measures of lung function — 1 second forced expiratory volume (FEV1) and forced vital capacity (FVC). FEV1 is the amount of air one can exhale in one second after taking a deep breath. FVC is the total amount of air one can exhale (for as long as exhalation lasts) after taking a deep breath. These measures are used, as well as their ratio (FEV1: FVC) to help diagnose lung diseases like emphysema and chronic bronchitis.
Initially, they found that the amounts of total adipose tissue (TAT) and visceral adipose tissue (VAT) were inversely and significantly associated with both FEV1 and FVC. Then, after about 3 years of follow-up, the measures were repeated. And, as shown in the figure below, as the amount of VAT decreased in men (blue circles) so did both FVC and FEV1; but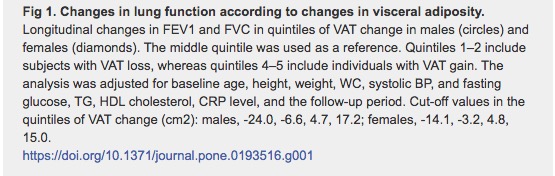 the same wasn't true for women. In contrast, the association between abdominal SAT and these measures of improved lung function were not significant. The authors suggested that the changes in lung function associated with decreases in VAT might be due to mechanical differences, e.g. less pressure on the diaphragm, and/or due to the greater propensity of the VAT to release inflammatory cytokines which could trigger systemic inflammation.
the same wasn't true for women. In contrast, the association between abdominal SAT and these measures of improved lung function were not significant. The authors suggested that the changes in lung function associated with decreases in VAT might be due to mechanical differences, e.g. less pressure on the diaphragm, and/or due to the greater propensity of the VAT to release inflammatory cytokines which could trigger systemic inflammation.
Thus, yet another aspect of the ill effects of obesity has been supported, and it will be important to replicate these results in other populations. Such data would be important in directing future clinical testing and treatment.




