The Spanish Flu of 1918, which caused a pandemic, is estimated to have killed about 2% of the world population, a death toll greater than the military deaths of World War I and World War II combined. Though they obviously would have lacked the technology and healthcare to do much about it, was there any way that public health officials could have foreseen that global plague?
Yes, possibly, suggests a new paper in the journal Annals of Epidemiology. A mostly mild wave of influenza cases early in 1918 could have served as a herald of the doom to come later that year.
In the northern hemisphere, flu season begins around October and lasts through March. But in 1918, what epidemiologists refer to as a "herald wave" of mild influenza cases occurred across the U.S., Americas, and Europe during the spring and summer. The moniker "Spanish Influenza" stuck because of the large number of cases in Spain.
What made the wave of influenza cases unusual was not only the timing but its high transmissibility. The basic reproduction number, R0, refers to the average number of people to whom one person will spread an infectious disease. Regular, seasonal influenza has an R0 of 1.2 to 1.5, but the herald wave had an R0 of 2.0 to 4.8. (By comparison, measles -- one of the most infectious diseases known -- has an R0 of 12 to 18.)
Another unusual feature of the early herald wave of influenza was the type of victim. The most severe cases typically occurred in young, healthy adults. Victims' skin would often turn bluish, and some patients' bodies were so ravaged by the disease that their lungs began to bleed. Sudden death was not uncommon and could occur within 24 to 48 hours of the onset of symptoms. There were even reports of people dying within four hours.
But those were the worst cases. Most influenza infections early in 1918 were mild. However, when autumn returned, and the influenza season was back in full swing, the Spanish Flu became catastrophic.
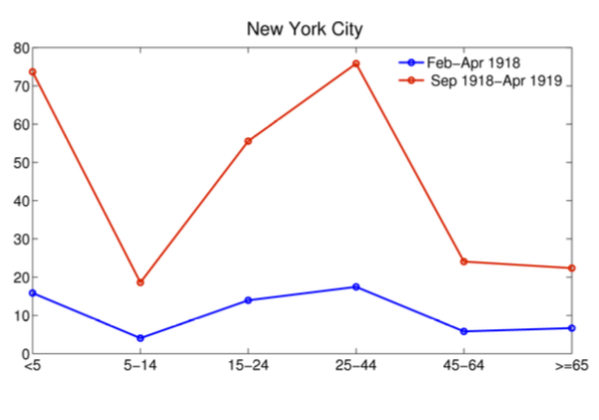 Once again, young people were hit particularly hard. The figure on the right shows excess mortality rates per 10,000 people in New York City from influenza in 1918. The early herald wave (blue line) was far less lethal than the autumn wave (red line). Note that people aged 15-44 were about two to three times likelier to die in the autumn wave (red line) than people aged 45 and older. This stands in stark contrast to seasonal influenza, which tends to kill older people.
Once again, young people were hit particularly hard. The figure on the right shows excess mortality rates per 10,000 people in New York City from influenza in 1918. The early herald wave (blue line) was far less lethal than the autumn wave (red line). Note that people aged 15-44 were about two to three times likelier to die in the autumn wave (red line) than people aged 45 and older. This stands in stark contrast to seasonal influenza, which tends to kill older people.
People who acquired influenza during the herald wave were quite lucky. The authors estimate that these people were 56% to 89% less likely to die in the fall, effectively "vaccinating" these survivors against the deadlier autumn wave.
The most compelling explanation for the unusual lethality pattern of the 1918 Spanish flu is known as the "recycling hypothesis." According to this hypothesis, older people were spared because decades earlier, they had been exposed to an influenza virus similar to the one that circled the globe in 1918. This hypothesis is supported by the fact that older people in isolated populations -- such as the native populations in Alaska and the Pacific Islands -- were not spared.
Beware the Herald Wave
In 2009, the world experienced another influenza pandemic, albeit far less lethal than the one in 1918. It is estimated that up to 203,000 people died, with most deaths occurring in younger people (i.e., people under the age of 65).
The authors conclude that "early pandemic waves of mild nature may in fact be the rule rather than exceptions." That may be useful information for predicting the next pandemic, a notoriously tricky task for epidemiologists. Those who come down with a mild case of the flu in the spring or summer may serve as a warning to the rest of us. Beware the herald wave.
Source: Lone Simonsen, Gerardo Chowell, Viggo Andreasen, Robert Gaffey, John Barry, Don Olson, Cécile Viboud. "A Review of Herald Pandemic Waves in 1918: Importance for Contemporary Pandemic Response Strategies." Annals of Epidemiology. Published online: March 2018. doi: 10.1016/j.annepidem.2018.02.013




