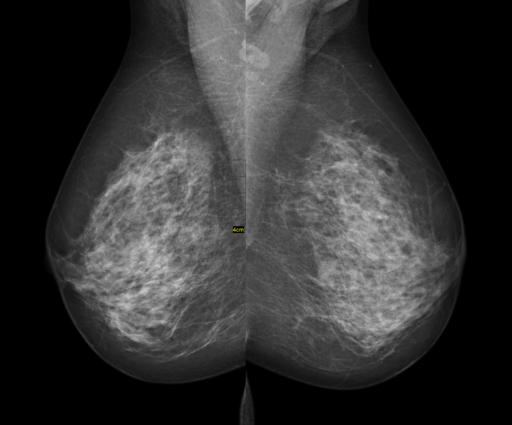
Mammography remains the standard means of screening for breast cancer. For women with denser breast tissue, the superimposition of tissue may mask early tumors even for the most observant of radiologists. A majority of states require the specific disclosure of breast density and the attendant possibility of falsely negative reports to patients. A study in Radiology takes a focused look at these patients using an automated measure of breast density rather than the subjective measures used in the US.
It is a retrospective, observational study of over 100,000 women and more than 300,000 mammographies contained in the BreastScreen database of Norway. Mammography studies were read independently by two radiologists who score findings on a 5 point scale. Those women with results other than normal, and this includes lesions described as “probably benign” or worse, are discussed and when deemed appropriate by the discussion, recalled for additional studies. The mean age of the patients described in the report is 58.3, and they underwent an average of 2.8 examinations during an 8-year study period.
Volumetric breast density was automatically calculated by the imaging software is analogous to the BI-RADS classification used in the US and had been shown previously to correlated “moderately” with BI-RADS. For this study, the two least dense groups were labeled “non-dense,” and the two higher categories of breast density were labeled “dense” breasts.
- 28% of women were identified as having dense breasts.
- The recall rate, a measure of disagreement between the radiologists, was 2.7% for non-dense women, 3.6% for those with denser breasts.
- Women with nondense breasts had fewer cancers identified initially (5.5% vs. 6.7%), and on interval examinations (1.2% vs. 2.8%) as compared to women with dense breasts, suggesting that breast density might be a marker for differences in a woman's physiologic responses.
- Once recalled, the treatment of women based upon breast density disappeared. 40.1% of nondense patients underwent needle biopsy; 38.9% for those with dense breasts. The yield of positive biopsies was also similar, 51% for non-dense breasts, 48% for those biopsies performed in dense breasts. [1]
- Tumors had smaller mean diameters and proportion of nodal involvement in non-dense breasts identified at the initial screening, but these differences were not found in tumors identified in interval examinations. This suggested that tumor growth, at least in the interval, was different for these two groups of women.
The recall rates were significantly less than 10% rate usually reported in the US and the authors attributed this to the independent readings by two radiologists. The authors point out that both the recall rate and biopsy rate was higher in women with denser breasts concluding that the higher biopsy rate resulted in higher cost. While I do not argue with the recall calculation, calculating biopsy rates based on all the women rather than those recalled seems incorrect; after all, no women underwent biopsy who had not been recalled. When the denominator for subsequent biopsy was adjusted to those recalled it seemed these women were treated identically and similar percentages of cancer identified. That means that the increased cost is related to the rate of recall, not the number of biopsies; the recall rates are a measure of radiologist's uncertainty.
Mammography is less sensitive in identifying the disease in women with dense breasts, the more than doubling of the rate of interval detection rather than initial discovery attests to that. Whether the less favorable tumor characteristics at interval discovery are due to the time interval or to some differences in the biologic behavior of cancer based upon breast density is unknown. What does seem increasingly clear though is that women with dense breasts are a separate subpopulation, their tumors are harder to detect and seem to behave differently. We need to consider ways to improve their screening - a practical means of personalizing medicine.
[1] I have recalculated the percentages from the paper using the actual numbers biopsied rather than the number of women screened as the denominator.
Source: Automated Volumetric Analysis of Mammographic Density in a Screening Setting: Worse Outcomes for Women with Dense Breasts Radiology DOI:10.1148/radiol.2018172972