Scottish journalist John Mackay published a study of crowd psychology in 1841 that speaks to the human impulse to believe any manner of nonsense if it plays into our emotional needs. Our minds are made up – don’t bother us with the facts.
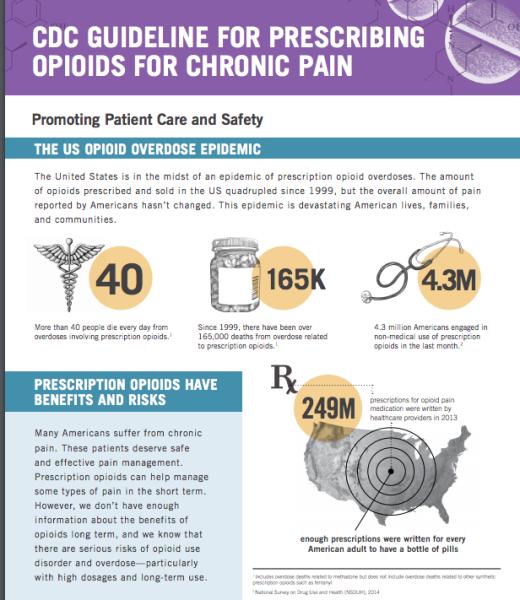
Mackay could have been describing our current “controversy” on prescription opioids and pain medicine. Media stories every day proclaim an “epidemic” of opioid addiction and overdose deaths. We are told that the cause of this disaster is over-prescribing of opioid pain relievers by careless doctors. Proposed remedies focus mainly on limiting patient access to prescription pain relievers.
Doctors are coerced to comply with such restrictions by ruinous “investigations” of drug enforcement authorities and State medical boards. Even when cleared of wrongdoing, such investigations have a ruinous impact on their financial wellbeing. It's no wonder that doctors are leaving pain management in droves. Thousands of clinics no longer accept new patients or deny treatment with opioid analgesics to all patients. Pain patients are routinely being abandoned relegating them to a life of agony, disability, and sometimes suicide when untreated pain becomes intolerable.
CDC Guideline on Pain
The primary cause of these atrocities is the 2016 Centers for Disease Control guideline on the prescription of opioids. As pointed out by dissenters and critics, CDC writers based their work on unproven or outright erroneous assumptions – not rigorous medical evidence.
The central doctrine of the CDC was that opioid dose – “Morphine Milligram Equivalent Dose (MMED)”, should become the measure of risk for addiction to pain meds. However, in November 2018, the American Medical Association publicly repudiated the use of MMED in setting practice standards.
In April 2019, CDC issued a “clarification,” claiming that their guideline was never intended as a mandate to restrict the availability of opioid pain relievers to people who need them. However, over 30 States had already weaponized the guideline into just such restrictions.
Also in April 2019, FDA issued safety warnings, noting that rapid or involuntary tapers may lead to patient destabilization and suicide. Six professional medical associations representing over half of all US healthcare providers went on record advocating for the removal of law enforcement from doctors’ offices. Yet still, doctors are being forced to choose between their own professional survival and the welfare of their patients.
Law enforcement officials and State Medical Boards continue to regard CDC Guidelines as the gold standard for prescribing practice. Authorities continue to tout key CDC assumptions that are clearly wrong.
Is Over Prescribing By Doctors Causing our Opioid Crisis?
In a word, no.
Published CDC data disprove this silly notion. In 2017, seniors over age 62 were prescribed opioids six-times more often than people younger than age 19. But the younger group suffered overdose-related mortality that was six times higher than seniors. Overdoses in seniors have been mostly stable for 20 years while skyrocketing among younger users. In no way can prescribing by doctors be claimed as a cause of overdose mortality.
Are Addiction and Overdose Common Among Medical Patients?
Again, no.
Dr. Nora Volkow, Director of the National Institute on Drug Abuse informs us that “addiction is not a predictable outcome of prescribing” and that addiction to physician-managed prescriptions is rare, even in people whose backgrounds suggest higher risk.
The Commonwealth of Massachusetts found that only 1.3% of people who died from an opioid overdose had a prescription for the drug found in their blood. Instead, deaths were dominated by illegal street drugs, often mixed with alcohol. In another study, of the North Carolina residents who were prescribed an opioid during one year only 0.022% (22 people per hundred thousand) died from an overdose.
In two studies of hundreds of thousands of post-surgical patients, fewer than 1% renewed their prescriptions longer than 13 weeks. Fewer than 0.6% were diagnosed with opioid abuse disorder within 2.5 years.
Are Opioid Analgesics Effective for Chronic Pain?
Despite claims of the guideline writers, there is evidence that they are. Due to high dropout rates among patients who were given placebos, the CDC writers found few long-term double-blind trials. CDC misinterpreted this lack as evidence of ineffectiveness. The agency also neglected to mention that long-term trials of non-opioid medicines and behavioral therapies are equally rare.
Are Safe and Reliable Alternatives to Opioids Available and Preferred?
Again, no.
Evidence for the effectiveness of therapies like chiropractic or acupuncture is very weak. No trials have compared opioid therapy directly to these alternatives. The most that can be said is that such therapies help some people with mild to moderate pain when added to analgesic drugs.
What’s Needed Now?
The CDC Guidelines on opioid prescribing must be withdrawn for a top-to-bottom rewrite. And it is essential that multiple patient advocates must be voting members of the panel
About the Authors: Dr. Lawhern is a technically trained non-physician patient advocate with 23 years of experience in moderating online patient support groups. Dr. Trescot is Board Certified in anesthesiology, addiction medicine, and interventional pain medicine. She is past President of the American Society for Interventional Pain Physicians.