A “catastrophic moral failure.”
Those are the words of WHO Director-General Tedros Adhanom Ghebreyesus asserting that “it’s unfair for younger, healthy adults in countries like the United States to get injections before the frail and elderly in poor countries.” Bruce Aylward, a WHO adviser, claims “it’s unacceptable for a country to vaccinate its entire population before offering doses to the highest-risk inhabitants of poorer countries.”
These assertions are premised on the bioethical principle of justice and the widespread belief that the elderly are most at risk. Thus, some claim that after vaccinating them and health care personnel, we should contribute our resources to those in similar need in impoverished nations. If these underlying assumptions are correct, perhaps there may be some validity to the concern that we would be vaccinating our younger-not-at-risk population while other at-risk suffer elsewhere.
However, there are two other bioethical principles to consider, beneficence (doing good) and non-maleficence (not doing harm), and they must be evaluated on a comparative basis, with full knowledge of the consequences. For whom should we be doing good? For whom should we be preventing harm? And are the mechanisms for effectuating both considerations the same?
We are really at the cusp of understanding COVID-19’s epidemiological predilections – let alone the mutant strains' behavior. What if we are wrong? What if the elderly are not the only ones significantly at risk? What if our younger population, the ones we would deny vaccines at home in favor of at-risk populations elsewhere, really should be our next concern? How does vaccination change COVID-19’s behavior?
COVID-19 in Israel
Pfizer was prescient in allowing Israel to be its guinea pig and provide what amounts to Phase IV data. Perhaps there might be lessons learned from the Israeli data. For example, these data may provide the first glimpse of what would happen if, once we’ve finished vaccinating those over 65, we shipped the rest to, say, South Sudan.
As of today, more than 30% of the Israeli population has been vaccinated with one dose; 20%% with two – 10% have received green vaccine certifications attesting to presumed immunity. These numbers include:
- 90% of those over 70
- 75% of those over 60
- Almost all nursing home residents, health care personnel, and younger persons with co-morbidities such as a history of cancer.
Early statistics indicate the effectiveness at a two-dose level is at 92%. The latest numbers suggest that “just .04% of Israelis were infected with COVID-19” being fully immunized with the Pfizer vaccine.
 Percentage Vaccinated by Age (Israeli Ministry of Health Dashboard)
Percentage Vaccinated by Age (Israeli Ministry of Health Dashboard)
Case numbers in Israel continue to grow – and grow dramatically
Yet, notwithstanding its early and aggressive vaccine rollout, which began on December 20, and a draconian lockdown policy (at a total of 139 days, Israel boasts the most prolonged lockdown in the world), 9.8% of all tests are still positive, among the highest since the pandemic began. The rates are attributed to either a high or low level of testing done that day, depending on the data du jour. On January 20 alone, 10,000 new cases were reported in a population of nine million.
Deaths, too, are increasing. More than 30% of all Israeli deaths were recorded in January – with 96 deaths reported for January 25, the highest single-day death rate since the epidemic began. The seven-day rolling average of deaths at January 28 was 61, also the highest since the epidemic began.
So, who is getting sick and who is dying? It’s not the oldest population, as statistics are beginning to confirm. And officials are stumped. If it’s not the elderly who are dying or getting sick, it has to be a younger segment.
“We are witnessing an increase in infections in women in the third trimester”
Prof. Galia Rahav, Director Sheba Medical Center
Infectious Disease Unit
School openings are supposed to be severely restricted (primarily open only to children of essential workers) – but pockets of resistance to government ordered school closures for the remainder exist within parts of the ultra-Orthodox communities where they remain open. And even when schools were allowed to be opened, 20% of students became ill. Country-wide, as of January 20, over 22,000 students and almost 3500 teachers were reported with active cases of COVID-19.
“a third of corona deaths in the first week of January were due to hospital overcrowding.”
Unsurprisingly, hospitals are overwhelmed. But the deaths are unrelated to age. Recent research reveals that the increase in workload may a factor leading to rising patient mortality.
The Israeli situation highlights the conflict between two goals in managing this pandemic: minimizing loss of life while stopping the spread. Minimizing deaths takes precedence, but if we cannot prevent the spread, the health care system cracks under the load – and becomes another risk factor for death.
Good policy needs good science
Without a complete understanding of the changing nature of the COVID-19 pandemic, we might be tempted to refrain from vaccinating the not-now-at-risk in favor of charitable work elsewhere. The Israeli experience suggests that would be self-destructive.
But more than self-destructive, failing to contain spread within a developed country would be just plain destructive from a world-health standpoint. (As they say on the airplanes, put your oxygen mask on first). Curtailing spread within a country is not only critical to maintaining a domestic health infrastructure; it is essential to prevent it from spreading outside a country.
Israel is now hermetically closing its borders – fearing import of the COVID-19 variant not from the third world, but rather from the highly industrialized nations with which Israel trades and shares tourists - those most likely to spread the disease to other countries. The best thing that wealthy countries might do for poorer countries is to prevent the infection from migrating there in the first place.
Good science needs good data. As for good intentions: do they lead to hell?
[Why should]“a healthy 20-year-old in New Jersey [get] vaccinated before a frontline health-care worker in South Sudan.”
Kate Elder, Doctors without Borders
The criticism still stings, so before rejecting the ostensibly charitable approach outright, let’s evaluate whether it would be acceptable public health policy to send vaccines to South Sudan.
South Sudan has a population of 14 million (3 million more than Israel and some six million less than New York)) As of January 29, South Sudan registered 3788 cases and 64 deaths (Compared to Israel, which has racked up over 4000 deaths, while COVID-19 claimed more than 43,000 lives in NY). Even without vaccines, the spread is far less, and the case-fatality is the same as America’s. But South Sudan has only four ventilators for the entire country. Sending in vaccines that will undoubtedly lose potency due to the need for sophisticated cold chain logistics would be rather injudicious – when the country could sorely use ventilators. Evaluating another country’s needs by a standard of what would be good for us seems rather paternalistic, about as tone-deaf as “let them eat cake.”
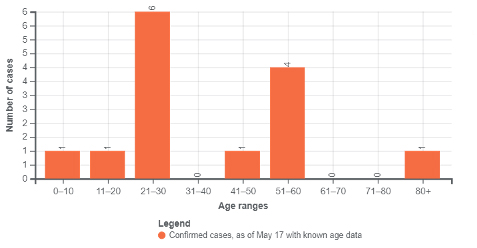
We would also need to evaluate who within South Sudan needs vaccination – who are those with the most significant risk? In South Sudan, the 21-30 year-olds are at the greatest risk, the same age group to whom we would deny vaccines in the US to enable our charitable donation abroad.
 Surely, addressing the needs of those disadvantaged is an ethical (benevolent) thing to do. But we have at-risk groups at home which need attention. The frail may not be able to access vaccines due to transportation difficulties; the Black and Latino population may need better explanations of risk; the impoverished may have financial issues securing vaccines. And the sooner we can contain spread in the developed world -the less likely we are to transport it to those in undeveloped countries.
Surely, addressing the needs of those disadvantaged is an ethical (benevolent) thing to do. But we have at-risk groups at home which need attention. The frail may not be able to access vaccines due to transportation difficulties; the Black and Latino population may need better explanations of risk; the impoverished may have financial issues securing vaccines. And the sooner we can contain spread in the developed world -the less likely we are to transport it to those in undeveloped countries.
Charity is a good thing. But as someone once said, charity begins at home.