Dr. Berwick and his co-authors enunciated the Triple Aim in a 2008 article in Health Affairs. [1] For many, it became, in the words of US News and World Report, the “North Star,” the marching orders for change. Perhaps it was only meant as an aspirational goal; the triple aim to expand care, improve quality, and lower cost remains elusive. Dr. Berwick doubles down in his latest opinion piece in JAMA. I was drawn to the article because it spoke of producing health. Producing? Sounds like health is some noun, an object turned out in a health system by providers. I tend to think of health as a verb or adjective.
It begins well enough, noting that our healthcare system is, in fact, designed to repair those with a disease rather than support and maintain our health. But then there is this,
“Genetics explains approximately 50% of the variation in health, whereas differences in health care account for an estimated 10%.”
With the exception of a few monogenetic diseases, I am unaware of studies showing that our genes are responsible for so much variation. Usually, I see single-digit percentages. But Dr. Berwick does provide a citation that we will return to in a moment. Here are the ten teams that all hospitals should “immediately establish” and link their leadership’s salaries.
- Health coverage - to achieve universal health care insurance coverage for the region served by the hospital.
- Food security - to end hunger and food insecurity.
- Housing security - aim to end chronic homelessness.
- Immigrant needs - to ensure excellent care and social support for all immigrants.
- Corrections and prison health - to foster a restorative and compassionate criminal justice system.
- Climate and decarbonization.
- Voting rights - to protect voting rights for all, including encouraging 100% voting for staff.
- Education supports - to strengthen elementary and secondary education in the region served.
- Early childhood supports - to help ensure safe birthing, early childhood support, and school readiness for all children younger than five years.
- Elderly and loneliness - to end social isolation for older individuals, which is associated with increased mortality and morbidity.
Quite the agenda for health systems that have had difficulties providing screening and preventative services during a pandemic. All of these are reasonable goals, and if not, at least goals we might consider. But are they the role of the health systems?
That brings us back to Dr. Berwick’s citation, County Health Rankings Relationships Between Determinant Factors and Health Outcomes, published in 2016 in the American Journal of Preventative Medicine. They analyzed the County Health Rankings, which evaluate every county in the US along 35 individual measures and two outcomes, longevity and quality of life. Here are their findings.
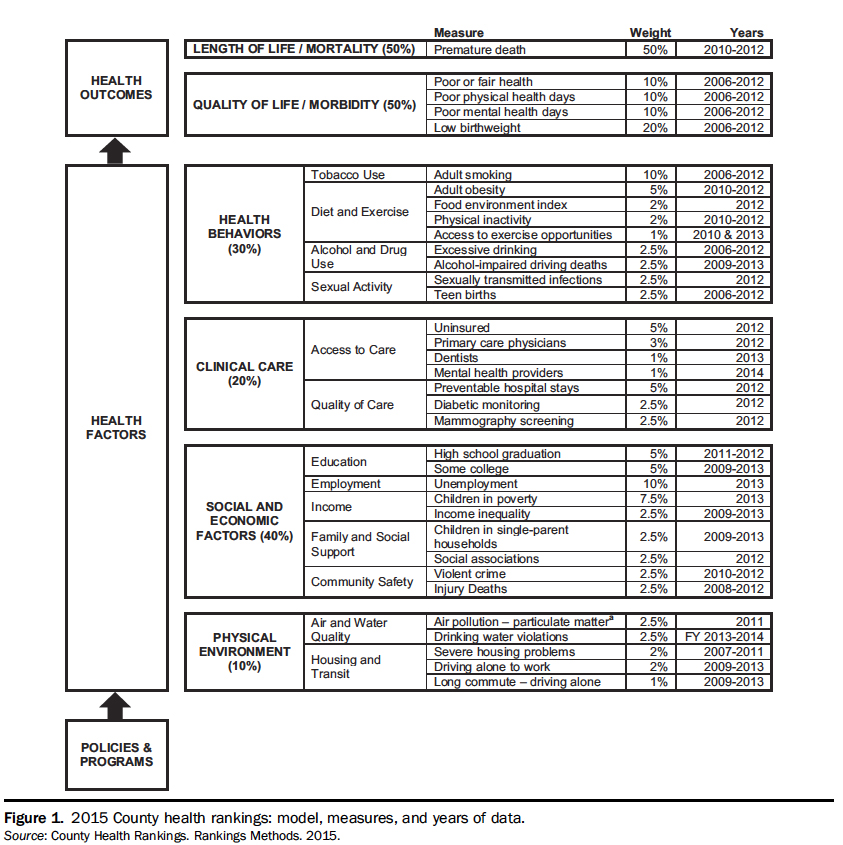
By my accounting, Berwick’s teams cover just about half of the social determinants of health found in his citation. Another 10% accrue to Triple Aims, now 14 years old and still not achieved. Food security, prison health, voting rights, and decarbonization were never considered by the County Health rankings, so their impact is unknown. But even if we were to move on them, what exactly is the regional or local health system to do?
Consider decarbonization, where Dr. Berwick again provides a citation. The most significant percentage of a hospital’s carbon footprint comes from the medications, devices, and packaging that flow through the supply chain into the care of patients. Most of that is single-use equipment, designed to reduce the need for local sterilization of reusables. One way to reduce single-use equipment is by “re-manufacturing” these devices; where an item is transported to one of several sites in the US, taken apart, some recycled, and some reused to rebuild the product. But even if you can convince physicians of the safety and quality of these “remanufactured” single-use items, their carbon footprint is still heavy.
How is the hospital going to provide housing or food security? As to voting rights, other than assuring that their employees have the times and means to vote, what rights can they provide?
Perhaps as before, Dr. Berwick’s words are meant to be aspirational. Maybe in a magical world, all those social determinants would be leveled. That of course would mean that the remaining variation in our health, 30%, is due to our behaviors. If the pandemic has taught us nothing else, we need to recognize that human behavior is an “error term” in most models (an unknown variable in the model), and that error term can be substantial.
[1] The Triple Aim: Care, Health, And Cost Health Affairs DOI: 10.1377/hlthaff.27.3.759
Source: Getting Serious About Producing Health JAMA DOI: 10.1001/jama.2022.6921