AvertD is “an innovative genetic risk assessment test” that utilizes genes associated with the brain’s reward pathways and addiction to assess the
“Genetic risk of developing OUD after taking prescription oral opioids for acute pain.”
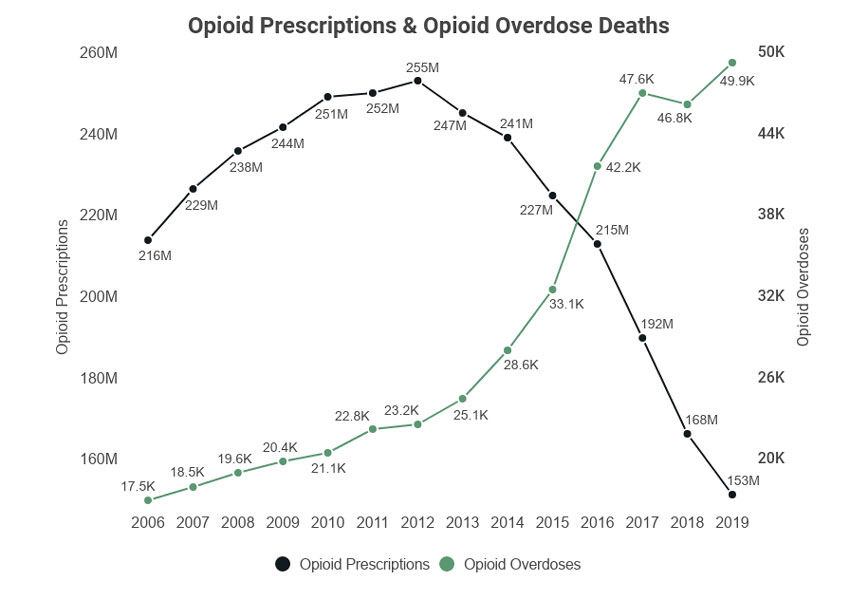
My colleague, Dr. Bloom, and his frequent writing partner, Dr. Jeffrey Singer, have written time and again on the misleading belief that our opioid crisis, whether we measure overdose deaths or individuals with opioid use disorder, is due to physicians writing valid prescriptions for opioids. According to the federal National Center for Drug Abuse Statistics, there is a clear inverse relationship between the number of opioid prescriptions written and overdose deaths, strongly suggesting that it is illegal, not prescription opioids are doing the real harm.
The intended market for the test is the 32% of individuals who receive an opioid prescription from a physician.
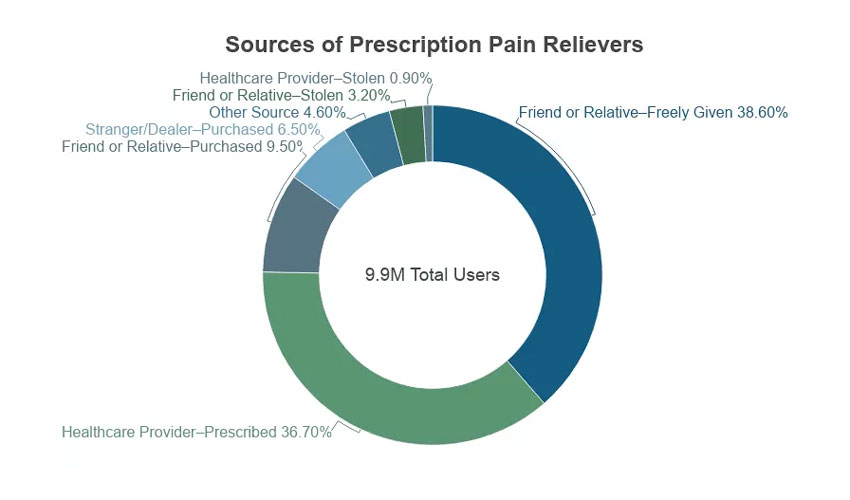 While the numbers may vary depending upon the source, roughly “1.9% of painkiller users say they are addicted,” and approximately 13% say they misused those prescription medications [1]. The presentation to the FDA by Solvd Health, the makers of AvertD, placed the number of individuals at risk for OUD at 1% of the population, about 3.5 million people.
While the numbers may vary depending upon the source, roughly “1.9% of painkiller users say they are addicted,” and approximately 13% say they misused those prescription medications [1]. The presentation to the FDA by Solvd Health, the makers of AvertD, placed the number of individuals at risk for OUD at 1% of the population, about 3.5 million people.
The AvertD Screen
The patient being tested has a swab taken of the inside of their mouth to collect their DNA, which is tested for “15 clinically relevant SNPs" [2] to identify patients at increased genetic risk for OUD. That information is given to the prescribing physician, who discusses the results with the patient in developing a treatment plan for pain management.
This was the second attempt to get FDA approval for this genetic screening test. It first failed to win approval 2-years ago because its ability to discriminate between those susceptible to OUD and those who were not was only as good as a coin toss. This time, Solvd Health presented data showing the test has an 82.8% sensitivity and 79.2% specificity – both measures of confidence in a diagnosis.
Sensitivity (True Positive Rate): The test correctly identifies 82.8% of the individuals with the condition. This means there is a 17.2% chance of a false negative result where the test fails to determine a risk for OUD.
Specificity (True Negative Rate): of the individuals who do not have the condition, the test correctly identifies 79.2% of them. This implies a 20.8% chance of a false positive result, where the test identifies a risk for OUD when none exists.
In practical terms, a more sensitive test may capture more true cases of the condition but at the expense of an increased likelihood of false positives. On the other hand, a more specific test may be better at avoiding false positives but could miss some actual cases. AvertD leans towards being good at identifying those with a genetic risk of OUD but may also flag some healthy individuals.
“Genetics Account for ~50% of a Person’s Risk for Drug Addiction”
I found that to be a rather startling percentage and took a moment to view the citations for this finding. Neither study made use of SNPs. The first was from a study of twin Vietnam veterans. The participants were all male, overwhelmingly White, and the finding of a 50% genetic underpinning for addiction was based on a model considering genetics, family environment, and nonfamily environment. They found that genetics was “responsible” for 50% of the use of heroin, not prescription drugs. Parenthetically, the same study indicated that genetics was responsible for 71% of marijuana use.
The second study, again in male twins, from the Virginia Twin Registry, found about 23% of opiate addiction was related to genetics and 64% to environmental factors. Marijuana addiction, by comparison, was felt to be 73% genetic.
While AvertD readily identifies the variable most resistant to change, our genetic risk, these citations make it difficult for me to accept that AvertD is measuring the most significant risk factor.
The Problems with Screening Tests
“AvertD is intended for use as a risk assessment tool – not a standalone diagnostic screening test – that should be used in combination with the healthcare provider’s assessment and evaluation of a patient.”
This is a bit of sophistry on the part of AvertD. It will be used for diagnostic screening to promote individualized care for those requiring opioids for “elective” acute pain –related to scheduled procedures or surgery. Given that the test will require a day or more to get results, it will not find an easy entry into the day-to-day prescription workflow of physicians treating “non-scheduled” acute pain.
In the data submitted to the FDA, the percentage of individuals with OUD was enriched, a technique used to help identify a “weak” signal. While the best of our guesses places the prevalence of OUD at a maximum of 13%, the percentage of individuals with OUD in the data submission was 4-fold more significant, 45%. This is a consequential difference. Knowing the specificity and sensitivity of a screening test is important, but it must be considered in the context of the prevalence of the condition being sought. The number of individuals with a false positive test, in this case falsely indicating a genetic predisposition to OUD, can be significant when the prevalence is low
If we were to consider 100,000 patients tested with AvertD where the prevalence of a genetic disposition to OUD was 1%, we would find [3]:
- True Positives (TP): 800
- False Positives (FP): 19,800
- True Negatives (TN): 79,200
- False Negatives (FN): 200
Even if we were to use the 13% prevalence, the number of false positives in that population would be 17,400 patients, all being counseled to avoid opiates in the mistaken belief that they have a genetic predisposition to misuse and addiction.
For those with an economic perspective, the test cost is $200. In the above example, we are spending $20 million to correctly identify 800 patients at possible risk for OUD, $25,000 for each patient identified. All of the AvertD data is retrospective; we do not know how many individuals will be identified, correctly or falsely, when the test gains greater adoption.
The second problem is knowing what to do with the information. The FDA was shown the following:
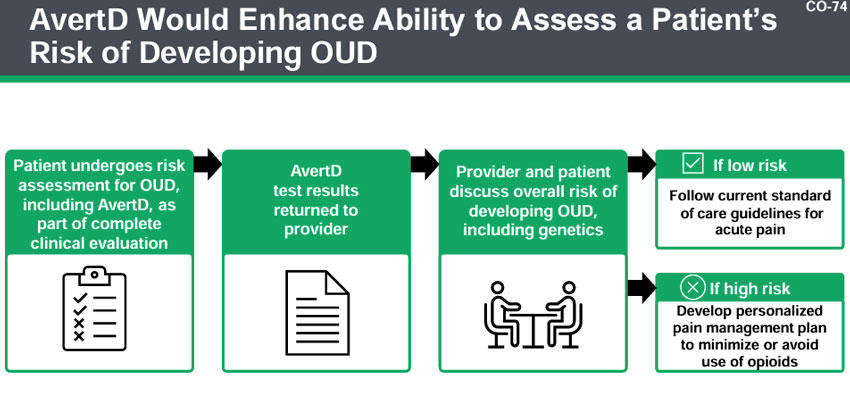
However, these are general guidelines; educational materials for training physicians and discussions with patients have yet to be developed. But the statement by Solvd Health, the developer of AvertD, on the harm of a false positive is revealing:
“Patient experiences emotional harm thinking he/she is at increased risk of OUD when they are not.”
Of course, they may also experience significant post-procedural pain.
As the test becomes a standard of care, its use and application will become a basis for malpractice litigation, litigation where the test is held blameless, but the physician, using the test or not, is the solely liable party. It is important that we find ways to make our health care more personalized or, as some say, more precise. But I am not sure that AvertD is as targeted as Solvd Health would lead us to believe. The FDA should require some post-market testing to demonstrate AvertD's real-world value.
[1] Misuse includes taking more medicine than you are supposed to in one dose, taking medication prescribed for someone else, taking medicine in a different way than you are supposed to, and using medicine for non-medicinal purposes. Two-thirds of those “misusing” pain prescriptions say they do so to relieve physical pain, suggesting that their misuse is more a problem of undertreatment. Only 11% of misusers use the prescriptions for recreation.
[2] SNP, or Single Nucleotide Polymorphism, is a common genetic variation among individuals. A wide range of studies have been used to associate various SNPs with diseases and traits.
[3] Number of individuals with the disease=1,000
Number of individuals without the disease=Total Population−Number of individuals with the disease = 100,000 − 1,000 = 99,000
True Positives (TP)=Sensitivity×Number of individuals with the disease = 800
False Negatives (FN)=Number of individuals with the disease − True Positives (TP) = 200
True Negatives (TN)=Specificity×Number of individuals without the = 0.8×99,000 = 79,200
False Positives (FP)=Number of individuals without the disease − True Negatives = 99,000−79,200 =19,800
Sources: AvertD Clinical Presentation to the FDA’s Clinical Chemistry and Clinical Toxicology Devices Panel
Co-occurrence of Abuse of Different Drugs in Men The Role of Drug-Specific and Shared Vulnerabilities Arch Gen Psych doi:10.1001/archpsyc.55.11.967
Specificity of Genetic and Environmental Risk Factors for Use and Abuse/Dependence of Cannabis, Cocaine, Hallucinogens, Sedatives, Stimulants, and Opiates in Male Twins American Journal of Psychiatry DOI: 10.1176/appi.ajp.160.4.687




