 via shutterstock
via shutterstock
The sequence of events required to keep the human heart beating for an entire lifetime is executed over two billion times. This occurs with near-perfect consistency, and a delay of even seconds can have serious implications.
A review article published in Trends in Molecular Medicine discusses the novel approaches based on stem cell technology and cellular reprogramming in potentially developing cells that can mimic the heart s natural pacemaker.
About three million people around the world have pacemakers, and each year about 600,000 new pacemakers are implanted, with a third of those patients receiving them in the United States. The most common indicator signaling a need for an artificial pacemaker is when the heart slows down and becomes incapable of adequately beating on its own. This condition prevents the body of meeting the demands of increased physical activity, and patients develop the following symptoms:
- Fainting
- Near fainting
- Dizziness
- Lack of energy
- Fatigue
- Shortness of breath
- Exercise intolerance
The heart s intrinsic conduction system is chiefly under the control of the sinoatrial node (SAN) where the electrical impulses are generated. It is comprised of a cluster of cells that sits at the apex, allowing for electrical currents to propagate through the rest of the heart. When these cells become diseased or malformed, conduction problems occur that can translate to death if not treated with the implantation of an electronic pacemaker.
Although lifesaving, electronic pacemakers are not devoid of complications. They are susceptible to infections as they are transplanted under the skin. Additionally, they have a limited battery life and may need replacing, thus requiring further surgery. There are other, very rare complications as well, making the prospect of biological pacemakers so exciting.
The SAN alone contains about 10,000 specialized pacemaker cells (PCs). Current research is attempting to trigger other areas of the heart that are not involved in the conducting process to acquire the ability to do so. Scientists are able to introduce genes that code for key conduction processes, reprogramming cells, to become electrically active whereas they were not before.
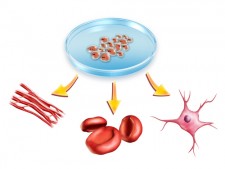
To take this a step further, strides are being made to replicate exactly the PCs in both their form and their function. This is where knowledge of developmental biology becomes paramount. Briefly, as an embryo develops in any species, cells become more and more specialized. Cells evolve from pluripotency to differentiated. Pluripotent cells can become anything. When they are differentiated they are permanently fixed in that role. Stem cells are pluripotent cells. If placed in any environment among other cells, neighboring cells will communicate with transplanted stem cells to tell them what to become and what to do.
Mapping the location of cells primed to become PCs allow them to be extracted and coaxed to differentiate into PCs in vitro. To be able to do this, however, requires an in-depth understanding of the embryo s microenvironment before it can be considered clinically viable.
Theoretically, biological pacemakers, which are composed of electrically active cells that can functionally integrate with the heart, could provide natural heart rhythm regulation without the need for indwelling hardware, said the author of the review, Vasanth Vedantham, of the University of California, San Francisco.
Biological pacemakers must meet a very high standard of performance to supplant electronic pacemakers. Because even a few seconds without a heartbeat can lead to serious consequences, a biological pacemaker would need to exhibit very robust and reliable performance," the author continued. "It remains to be determined whether this will be technically feasible. Despite such challenges, the field is poised for rapid progress over the next few years.



