High blood pressure, hypertension, is a pervasive health problem in the U.S. and globally. It consumes significant amounts of health dollars and is a co-morbidity or risk factor for many of the chronic diseases that ‘plague’ Western society. Given all the costs and concerns you think we could easily describe the natural history of the onset of hypertension, Because we tend to think in moments rather than longitudinally high blood pressure is defined as crossing some, arbitrary and often controversial threshold (the current guidelines are 130mmHg for the systolic, or upper number). A recent paper in JAMA provides insight into the dynamics of hypertension’s onset. It is not as cut and dried as our numerical threshold suggests.
In the static model, one day you are normal, the next hypertensive – after all, you have only two points in time to compare. Although there are rare causes for the abrupt onset of hypertension, for a majority of cases this binary, one day normal, the next hypertensive, makes little physiologic sense. Because we only diagnostically acknowledge passing the threshold we are left to imagine, the scientific word choice would extrapolate, how those two points connect. We have assumed a linear model, a straight line connecting the two points, a blood pressure changing at a constant rate over time. But in fact, the researchers found that blood pressure, once it passed a threshold value, rose fairly rapidly towards the diagnostic threshold consistent with clinical hypertension. The onset of hypertension, as it turns out, is more S-shaped than a straight line. A quick look at the data and then a consideration of what it might mean.
The Study
1252 individuals, from the long-term Framingham study, age 40, without a clinical diagnosis of hypertension, had an aggregate 16,072 blood pressure measurements collected at two-year intervals. The mean age was 35.3 at the time that the blood pressure determinations were initiated and about 60% of the cohort were women. I will not belabor the individual numbers, but in essence, blood pressure was maintained between 120-125mm Hg for long periods of time, but once crossing this threshold, rapidly (if every two years is a good measure of rapidity) rose into hypertension’s diagnostic category, in this case the older 140mmHg. Here is the associated graphic.
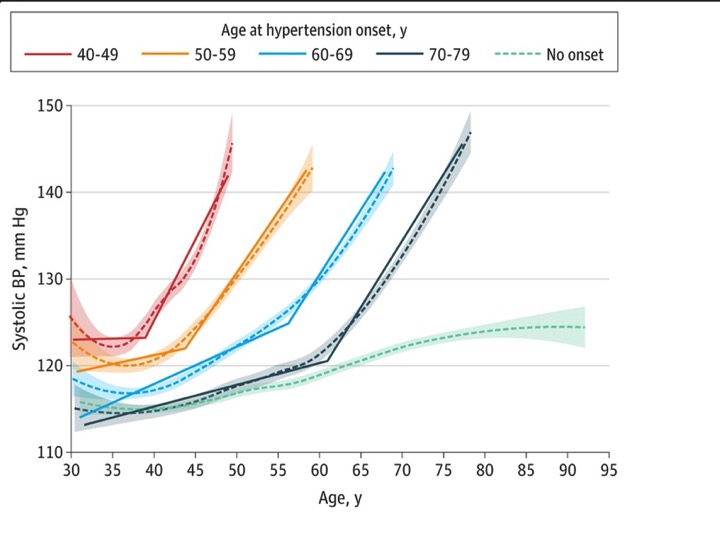 While the age of hypertension's onset varied, the pattern of relative stability giving way to rapid changes creating an S-shaped sinusoidal curve, rather than a linear rise, appears unmistakable, at least qualitatively.
While the age of hypertension's onset varied, the pattern of relative stability giving way to rapid changes creating an S-shaped sinusoidal curve, rather than a linear rise, appears unmistakable, at least qualitatively.
Based on this more longitudinal view the researchers recommended that 125mm Hg be considered as a measure of “pre-hypertension” and that more active surveillance be initiated. They rightly believe that while medication is not warranted, non-medical measures, like diet or stress reduction might be implemented.
Musings
Any number of articles have discussed pre-this or pre-that and have recommended increased vigilance and supportive measures. So I do not believe the value of the study is to found in those medical homilies. I am far more interested in the seemingly dramatic inflection point, let me call it a phase transition. Why after a period of little change, does our blood pressure begin to rise? Our blood pressure is, for the most part, maintained within a homeostatic range. But should we substitute the word resilience for homeostasis, the rise in blood pressure over time reflects a loss of resilience - we are no longer able to cope with whatever factors are causing our pressure to rise. To continue the analogy, when the balance of cause and restoration has tipped further away from restoration, we require medication to augment our failing physiologic reserve.
The fact that hypertension begins at so many different ages (phenotypically heterogenous) merely reflects that for each of us cardiovascular resilience varies. By considering hypertension a marker of declining cardiovascular resilience, it means the static definition of high blood pressure as a risk factor is inaccurate. It means that the clinical problems we collect over time both interact with one another and have a common pathway, as an increasing loss of resilience to our vital systems gives way to frailty and our deaths. The value in this study is to nudge our thinking and conception of health towards dynamic, longitudinal views, away from the static snapshots we have found on the annual physical examination. Static cross-sectional studies are far easier to do but may not give us as accurate a picture of our health.
Source: Trajectories of Blood Pressure Elevation Preceding Hypertension Onset JAMA DOI:10.1001/jamacardio.2018.0250




