High blood pressure, hypertension, is a pervasive health problem in the U.S. and globally. It consumes significant amounts of health dollars and is a co-morbidity or risk factor for many of the chronic diseases that ‘plague’ Western society. Given all the costs and concerns you think we could easily describe the onset of hypertension in more of a dynamic way compared to simply saying once your blood pressure is higher than 130 mm Hg for the systolic or upper number, the current guideline, you are hypertensive. A new paper in JAMA describes the onset of hypertension; it is not a static, yes-no, process.
In the static model, one day you are normal, the next hypertensive – after all, you have only two points in time to compare. This makes little physiologic sense, so we are left to imagine, the scientific word choice would be extrapolate, how those two points connect. We have assumed a linear model, with the blood pressure slowly changing over time. But in fact, the researchers found that blood pressure, once it passed a threshold, rose fairly rapidly into the criteria consistent with a diagnosis. First, a look at the data and then a consideration of what it might mean.
Study
1252 individuals, from the long-term Framingham study, age 40 without hypertension had an aggregate 16,072 blood pressure measurements collected at two-year intervals. Mean age 35.3, about 60% women. I will not belabor the individual numbers, but in essence, blood pressure was maintained between 120-125mm Hg for long periods of time, but once crossing this threshold, rapidly (if every two years is a good measure of rapidity) rose into hypertension’s diagnostic category, in this case, the older 140mmHg. Here is the associated graphic.
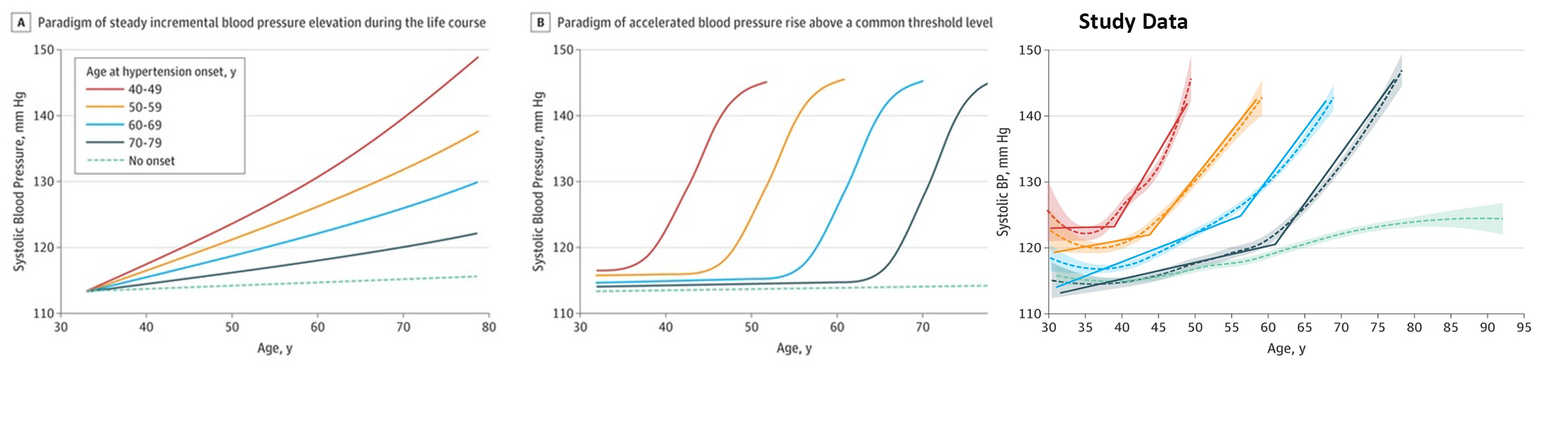 While hypertension remains a heterogeneous disease, with varying ages of onset and subsequent differing severity, the pattern of relative stability giving way to rapid changes, a sinusoidal curve, appears unmistakable, at least qualitatively.
While hypertension remains a heterogeneous disease, with varying ages of onset and subsequent differing severity, the pattern of relative stability giving way to rapid changes, a sinusoidal curve, appears unmistakable, at least qualitatively.
Why the pattern of change?
I think the most critical question is why the change, the phase transition, has this particular trajectory? Our blood pressure rises and falls, for the most part, maintained within a range – an aggregate of multiple, interacting environmental (e.g., stress) and physiologic (e.g., narrowing of our blood vessels) factors. If one factor were “the cause,” then the trajectory of change would be linear.
The sinusoidal shape suggests that while one component may be predominant, the body is capable of mitigating those declines. For example, stress may raise your blood pressure, but supple arteries capable of dilating can quickly return the blood pressure to the normal range. But as the arteries become less flexible, due to atherosclerosis, they may not enlarge as rapidly or as much, and your blood pressure doesn’t return all the way to the normal range; you are less resilient. In complex systems, small changes in multiple variables all changing at their own rates can aggregate producing that sinusoidal trajectory. There is no single cause for hypertension it is the result of many small changes and interactions we have not being able to describe adequately. Hypertension has a unique path for each individual.
There are many ways up a mountain, some easier than others, but the path is as important as the summit. Taking one route over another may leave you more exhausted and less able to climb the next peak. Analogously, I would argue that the patient that has hypertension and then diabetes may be different than the patient that has diabetes and then hypertension, that pathway matters. When we think of hypertension as a risk factor, a static, monolithic phenotype, we lose the nuance of the path. When we treat multiple diseases as fixed risk factors simultaneously, the information to be learned from the varying pathways is lost in the aggregation; making our clinical models less accurate and contributing to contradictory or paradoxical findings. We need to recognize that in dynamic systems, pathway matters.
Source: Trajectories of Blood Pressure Elevation Preceding Hypertension Onset JAMA DOI:10.1001/jamacardio.2018.0250




