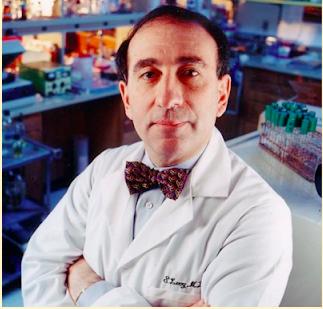
Dr. Stuart Levy, a giant in the world of infectious disease, passed away last week. ACSH advisor Dr. David Shlaes, a former colleague of Dr. Levy (pictured), examines his legacy.
Stuart Levy passed away last week after a long illness. He was a friend, not a close friend, and a colleague. I hadn’t spoken with him in a while – probably not since I wrote an article for the Alliance for the Prudent Use of Antibiotics (that he founded) Newsletter last year. But I think I speak for many when I say that I will miss Stuart.
I first met Stuart in the mid-1980s, just after I started my career in infectious diseases. He was one of a number of antibiotic-resistance researchers who were complaining that the NIH was not funding their research. I joined this group of “disgruntled” scientists, as Science magazine referred to us in a 1994 article, and got to know Stuart well. He was a leader of our effort to try and hold the NIH accountable. We felt that our grant requests were not being reviewed by our peers, but rather by experts in areas such as vaccinology, immunology and pathogenesis. Our group included greats in the area like George Jacoby, Bob Moellering, Gordon Archer and several others. Stuart was instrumental in getting the NIH to provide data on their past funding for antibiotic research (nil) and for helping to arrange a series of workshops with NIH to explore the reasons for this lack of funding and lack of appropriate peer review. He was the diplomat of the group. The NIH finally followed Stuart’s advice and established a separate study section to deal with antibiotic research 20 years after Stuart first suggested the idea.
When I met him, Stuart corrected my misguided assumption that he was a microbiologist or an infectious diseases specialist. He pointed out that he was a hematologist in a department of hematology and oncology. I understand my mistake as I look back on his career. He was probably the first or one of the first to demonstrate the effect of antibiotic feed supplements for animals on the emergence of resistance in farm animals and the transmission of that resistance to humans in the farm environment. He developed the notion that antibiotics follow the “you use it, you lose it” rule, and that using them more sparingly might delay the emergence of resistance. He was a strong believer in the idea that the density of antibiotic use was correlated with the rapidity of emergence of resistance. He founded the Alliance for the Prudent Use of Antibiotics in 1981 with the goal of protecting that precious resource.
In the late 1990s, Stuart was part of a large group working on guidelines for the Infectious Diseases Society of American and the Society for Healthcare Epidemiology of America for the prevention of resistance in hospitals. This turned into a two-year effort where I became the secretary for luminaries like Stuart, Dale Gerding and John McGowan. Stuart and the others pushed hard for systems to control the use of antibiotics in hospitals with the goal of slowing emerging resistance. In the guidelines that were finally published, this became known as antimicrobial stewardship and achieved prominence both then and now.
Stuart also pointed out the potential importance of antibacterial products used in homes and industry for everything from hand washing to environmental cleaning. He realized that resistance to these products was often related to augmented bacterial efflux and that this efflux could affect the activity of standard antibiotics as well.
In later years, I used to quibble with Stuart by noting that even appropriate use of antibiotics, as is the case for most hospital use these days, will select for resistance. He would always counter with his density of use argument.
Stuart also was prominent in showing us that commensal bacteria could be important harbingers of resistance genes for pathogens. Thus, antimicrobial use of any kind could provide selective pressure on the commensal flora that, in turn, could pass on acquired resistance determinants to any pathogens in the same niche. He noted that the problem was that we did not routinely survey these commensals, but rather focused on the pathogens.
Stuart was a tetracycline researcher. Not only did he discover various tetracycline resistance determinants, but he also founded a company (Paratek) that competed with Wyeth in the development of new tetracycline analogues. I remember this well since I worked at Wyeth where tigecycline was our major project at the time. During Stuart’s work on tetracycline resistance, he came upon the Mar system that was involved in the early steps towards multiple antimicrobial resistance as well as being important in virulence and the response to environmental stress in bacteria.
I always considered Stuart a friend and a mentor. I am personally saddened by his passing. There are few with the depth and breadth of knowledge combined with an ability to move others to act that Stuart possessed. We will all miss him.
Category



