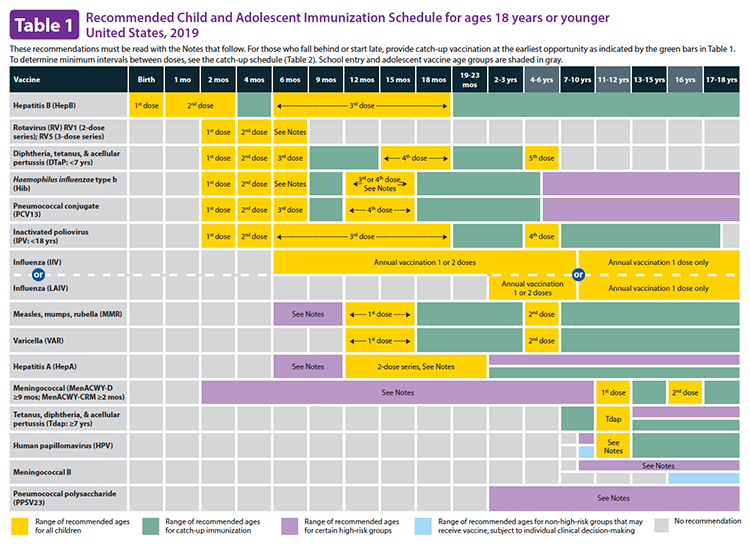
Anti-vaccination advocates hold many beliefs, from the thoroughly discredited allegations of Dr. Wakefield to concerns that vaccination somehow abridges religious freedom. During the first year of life, the CDC, in conjunction with advisors from the American Academy of Pediatrics Committee on Infectious Diseases, recommends ten different vaccines. Here are the CDC immunization recommendations for children, from birth to 18 years of age.
For some parents, common sense tells them that this is too many, and they should be spread out. Of course, common sense also tells us the earth is flat and that the sun revolves around the earth. But they can raise an important question, are vaccination schedules evidence-based?
The short answer is no, the longer answer is more nuanced and centers around distinctions between evidence-based from evidence-informed – a distinction that confuses most readers of guidelines.
What is the scientific evidence?
First, let’s leave no room for anti-vaxxer conspiracy theories. Vaccines are licensed for use only after randomized controlled trials demonstrating their safety, ability to create an immune response (immunogenicity), and their effectiveness in preventing the targeted disease.
In the early 1950’s, 15,000 of our children were paralyzed from polio and the value of the Salk vaccine proven when 1.3 million children underwent a randomized double-blind control study. In 2018, there were 33 cases of polio globally [1]. You cannot get better evidence that treatment results in better outcomes. Additional studies “generate critical data regarding age-specific immunogenicity, dose and dosing intervals, interaction with other vaccines, duration of immunity, and overall vaccine safety to inform schedules.” [Italics added]
Determining a schedule involves knowing more than the efficacy of a particular vaccine. It requires identifying which diseases are threatening and when – an assessment of the epidemiology of each “disease threat.” The behavior and characteristics of the viruses and bacteria are not static; they change in relation to their environment, which includes our reactions to them. For example, antimicrobial resistance; or global travel by jets that allow measles to hop from one country to another in a day.
Determining a schedule of vaccinations involves logistics. At the manufacturing level, it requires coordination in producing the right amount of the right vaccine at the right time. It takes five to six months to provide sufficient viral vaccines, which is part of why the efficacy of the “flu shot” varies annually – we have to take our best guess far in advance of which influenza strain to guard against.
Of more significant logistical concern is that coming in every month for immunization is disruptive to children and parents. In high-income Western countries, “the lower risk of acquisition of many infectious diseases and better access to care permit vaccination to be incorporated into established well-child visits through the first six months of life.” In central Africa, where epidemiology suggests an “early burden of vaccine preventable diseases,” and getting newborns to physicians is more difficult, the schedule is more contracted. To paraphrase former Speaker of the House, “Tip” O’Neil, all immunizations schedules are local.
If you look at the contemporary history of vaccinations, they came along one after another. While they might have been helpful, there was no randomized controlled study demonstrating that one schedule of immunization was better than another. Even critics of immunization schedules admit that “the time for such studies is ethically and logistically past.” There will be no randomized controlled studies. In their absence, we must marry and merge our best epidemiologic, logistical, and cultural knowledge. We need to connect the dots
Connecting the Dots
There is a group tasked with connecting the dots. The Advisory Committee on Immunization Practices of the CDC includes “expertise in vaccinology, immunology, pediatrics, internal medicine, nursing, family medicine, virology, public health, infectious diseases, and/or preventive medicine; one member is a consumer representative who provides perspectives on the social and community aspects of vaccination.” (You can find the list here.)
In the absence of studies of immunization schedules, their expertise and judgment inform the process. Immunization schedules are grounded in the science of epidemiology, and the practicality of logistics into an immunization, the schedule the creation of science-informed judgment.
In healthcare, evidence-based care is an aspirational goal. But evidence-informed care, as our immunization schedules have demonstrated, can be just as helpful in preventing disease.
[1] An excellent timeline of polio vaccinations can be found here.
Source: Is the timing of recommended childhood vaccines evidence based? British Medical Journal DOI:10.1136/bmj.i867 and “Are the recommended childhood vaccine schedules evidence-based?” Science-Based Medicine