The health system wants you back and rather than dwell on cash flow and other financial vagaries, the discussion is all about how the COVID-19 instituted delays, may further harm your general well-being
"For patients with cancer, delay of surgery has the real potential to increase the likelihood of metastatic disease, with some patients' tumours progressing from being curable (with near normal life expectancy) to non-curable (with limited life expectancy)."
With that opening, consider this paper, Collateral Damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. From the title and that opening statement, I anticipated a lot of collateral damage – spoiler alert, as with everything else, the loss is unevenly experienced.
The researchers made use of data in the Public Health England National Cancer Registry for the years 2013-17. Using those numbers and a large number of assumptions about surgical complications, possible life-expectancies, they created a model of how delays in care would, through the progression of the disease, result in more deaths and shorter life-spans. Despite having data for only three cancers, they extrapolated their findings to many more.
Remember, it is a model, and its functionality lies in showing the relationship between variables. The numbers are at best guesstimates, while the media may highlight them to get your attention, they bear only a tenuous connection to reality.
With the preamble out of the way, here is what they found.
- "The greatest rates of deaths arise following even modest delays to surgery in aggressive cancers, with over 30% reduction in survival at six months and over 17% reduction in survival at three months…"
- "…for cancers with a relatively good overall prognosis, delay of surgery by three months had a minimal impact on survival: <1% for all Stage 1 ER+ and HER2+ breast cancers, for example."
Let me rephrase, for those patients with imminently life-threatening cancers, delay in treatment resulted in shorter life-expectancy. For those with less aggressive cancers, the kind that comes with five year or longer survivals, the delay had little impact. Another way to produce a big, attention-grabbing number is to calculate years of life lost or gained – life-years. [1]
- "Prior to the COVID-19 crisis, each year cancer surgery was directly responsible for 1,717,051 LYGs. This represents, on average, 18.1 LYG per patient, which markedly reduces to 17.1 with three months' delay and to 15.9 with six months' delay."
Don't let those numbers be overly concerning for two reasons. First, that year lost with a three-month delay, and 2.2 year loss with a six-month delay is an aggregate, the consequence of delay fell primarily on those with only a short life-expectancy. Second, the model also considered how COVID-19 impacted our life years and came to an unexpected conclusion.
"It is therefore noteworthy, that a delay of surgery by six months results in 208,275 lost life years for an annual quota of surgical patients: this equates to 43% of the total 482,022 life-years gained from hospitalisation of an equivalent number of community-acquired COVID- 19 cases."
Yes, you read that correctly, treating COVID-19 patients in place of those with untreated cancers resulted in a net saving of life-years, almost 60% more. So again, while the numbers seem real and aren't, the trend is more than likely correct. While some patients, with advanced cancers, may experience a loss of several, very important months of their lives, from the public health perspective, delaying cancer care to care for COVID-19 patients was the right move.
The researchers go on to make two salient recommendations.
- Because of the risk of hospital-acquired COVID-19, especially in older patients undergoing initial cancer surgery, hospitals should segregate patients, creating "cold-zones," which I presume to mean areas with heightened partitioning from COVID-19 patients.
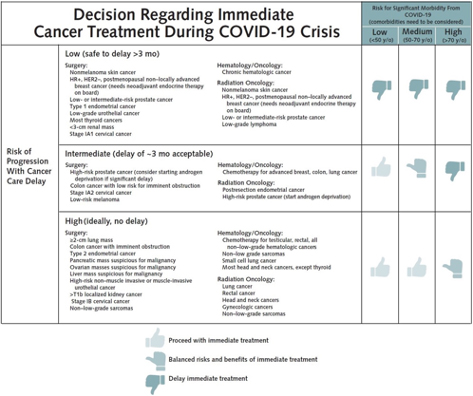
- As the backlog of patients requiring care is addressed, priority should be given to those with aggressive tumors who are young enough to have significant gains. For patients with slower-growing tumors, the back of the line may not result in less anxiety, but it does not seem that it will lead to substantially worse outcomes.
Here is a graphic of their triage tree.
[1] Basically, you calculate the individual years gained or lost multiplied by each individual and then aggregated.
Source: Collateral Damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic Annals of Oncology DOI:10.106/j.annonc.2020.05.009




