Despite the massive increase in COVID-19 testing, the reality is that tests are in limited supply. Pharmacies in several cities have implemented a screen to determine who can or cannot get a COVID test. Those who are unlikely to be infected with the coronavirus aren't given a test.
Because demand perpetually outstrips supply, there needs to be a way to discriminate between people who likely have COVID from those who do not. To that end, a team of scientists led by Saar Shoer and Eran Segal published a study in the new journal Med that determined that the answers to nine simple questions can predict with 74% accuracy whether somebody has COVID. The nine questions are:
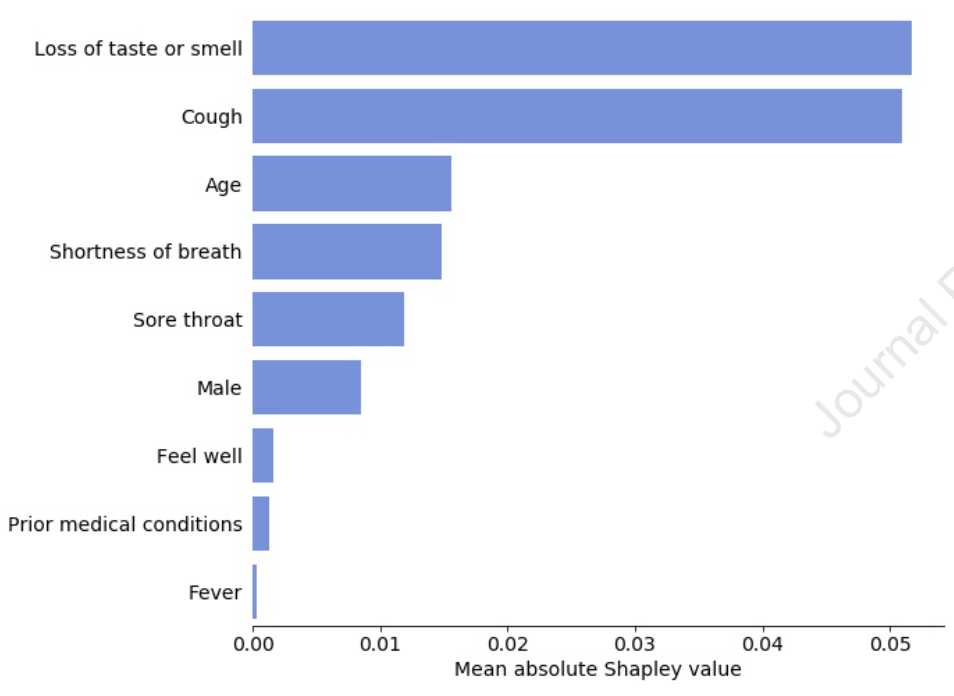 Have you lost your sense of taste or smell?
Have you lost your sense of taste or smell?- Do you have a cough?
- How old are you?
- Do you have shortness of breath?
- Do you have a sore throat?
- Are you male?
- Do you feel well?
- Do you have prior medical conditions?
- Do you have a fever?
As shown in the figure, the first two questions were the most relevant at determining whether someone is likely to be infected with the coronavirus. Also, older people and males were more likely to have COVID than younger people or females.
Their results are important not just for the allocation of scarce resources. Diagnostic tests are imperfect. No matter how good they are, all tests produce false positives and false negatives. This means that a person who tests positive may not actually be infected, while a person who tests negative might actually be sick. The likelihood of getting an accurate test result increases if the person getting the test has been pre-screened.
Another paper by Edward Stites and Craig Wilenin the same issue of Med elaborates. See the graphic below.
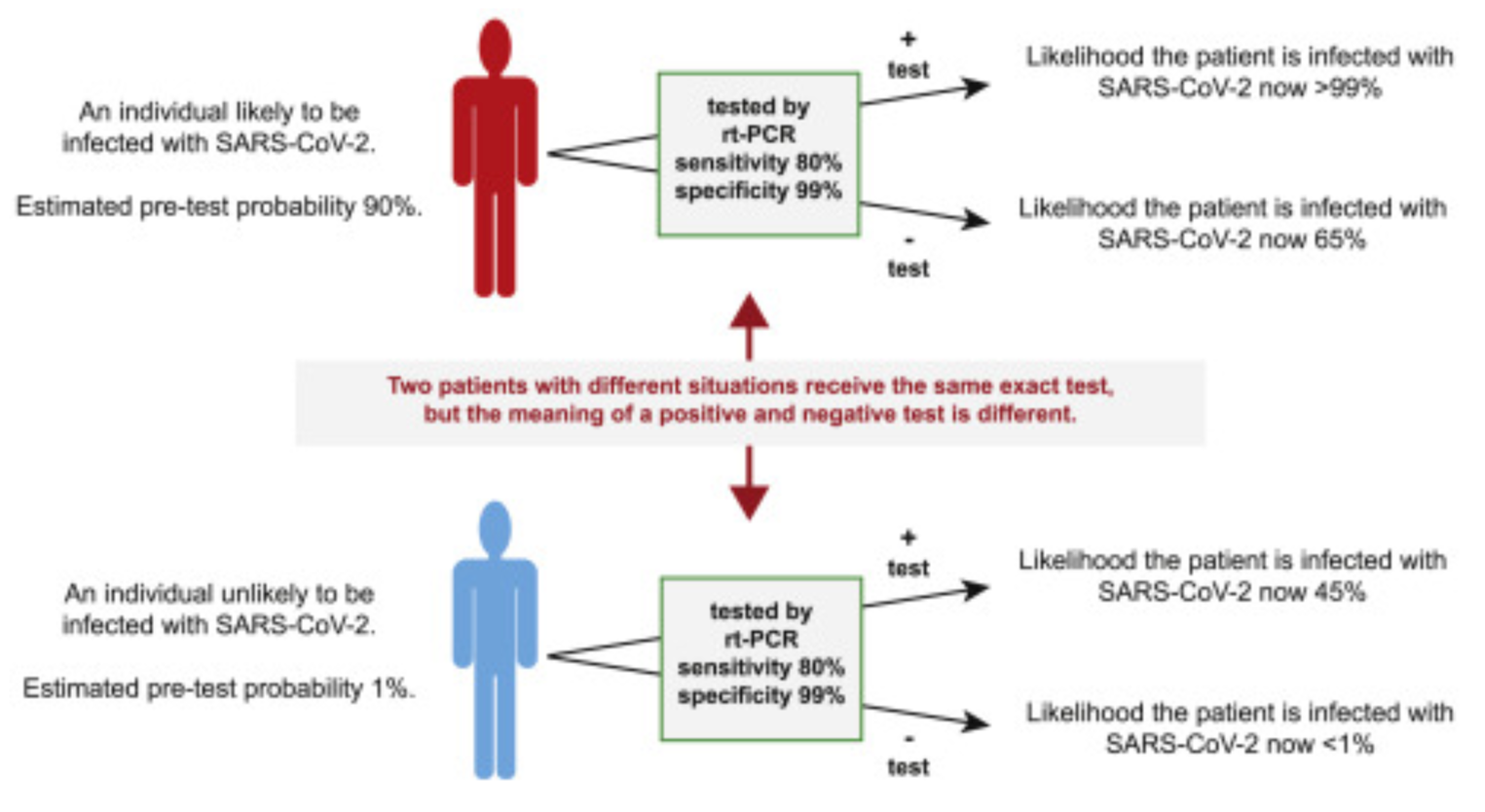
The image depicts two scenarios. In the first, a pre-screened patient is deemed likely to be infected. In the second, a pre-screened patient is deemed unlikely to be infected. If they are both given the same diagnostic test, which in this example has a sensitivity of 80% and a specificity of 99% (for a review of these terms, see this article), the likelihood that the test results truly reflect reality improves.
In the upper panel, the pre-screen gave the patient a 90% likelihood of being infected. After the positive test result, the likelihood that the patient really does have coronavirus is greater than 99%. (If the patient tests negative, he is still about 65% likely to have the disease, given the pre-screen results.)
In the lower panel, the pre-screen gave the patient a 1% likelihood of being infected. After the negative test result, the likelihood that the patient is sick is less than 1%. (If the patient tests positive, the likelihood of infection is 45%.)
Combined, these papers show that asking the right questions combined with a good diagnostic test can greatly increase the accuracy of test results. In a fast-moving pandemic, accuracy is priceless.