The data causing concern comes from the UK’s Public Health England’s dataset in a report by the Scientific Advisory Group for Emergencies (SAGE). The same data was reviewed by two groups, using different statistical methodologies.
The London School of Hygiene & Tropical Medicine (LSHTM)
- There were 2,583 deaths among 1.2 million tested individuals. 384 had the B.1.1.7 variant.
- When adjusted for age, gender, co-morbidities, and geographic location, the B.1.1.7 virus was 35% more likely to result in death.
The Imperial College of London
- They measured differences in outcome two ways; based on case fatality rates and using a control group weighted to reflect the characteristics of individuals infected with B.1.1.7.
- While the two results varied, once again, they found that B.1.1.7 was 29 to 35% more likely to result in death than “normal” COVID-19.
Public Health England
- They looked at 92,207 B.1.1.7 cases along with a matched cohort.
- The odds of hospital admission were not significantly different for the variant
- There were few deaths in both groups, but B.1.1.7 had a rate of 0.09%, while that of the original strain of COVID-19 WAS 0.07%. This absolute difference of 0.02% represents a relative difference of 28% - consistent with the two other studies. While both numbers reflect the same differences, one is much larger and scarier, the relative difference. Relative difference is what is getting all the ink, digital or real.
- In a retrospective review, patients were followed for one month after a positive test. When the time period was earlier in the pandemic, the mortality of B.1.1.7 and COVID-19 was identical. The same study performed on patients later in the pandemic indicated that B.1.1.7 increased mortality by 65%. Data reporting lags so that the time frame of sampling matters in the completeness of the information. Importantly, the behavior of B.1.1.7 differs as it reaches different hosts much like the age-related mortality we see with the original strain of COVID-19. The virulence of B.1.1.7 is not static.
The Caveats
- Most importantly, this data reflects a very small subset of deaths. Only 26% of COVID-19 deaths have PCR confirmation (what the English call Pillar 2 testing), and of those, only 30% have a determination of the S genes status. We are looking at only 8% of the deaths during this period.
- Statistically, carrying the data out to 28 days from diagnosis resulted in a loss of statistical strength and “removed the excess death signal.”
- If there is an increase in severity, it is not apparent in increased hospitalization for B.1.1.7. Further, after adjusting for date of admission, age, gender, co-morbidities, and ethnicity that has been no reported increases in hospital-based mortality.
- As with much of our COVID data, there are lag times and missing case information that makes the data less certain or complete. As the report notes, “Restricting the analysis to a trust [health region/system] with a high proportion of proven VOC [variants of concern] … found no statistically significant change in hospital case fatality rates comparing proven VOC with non-VOC cases.” Of course, that sentence comes with the disclaimer that those VOC cases may have died at home.
The Conclusion
“There is a realistic possibility that VOC B.1.1.7 is associated with an increased risk of death compared to non-VOC viruses.”
Unlike other agencies, SAGE quantifies what they mean by saying “realistic possibility.” Here is the graphic.
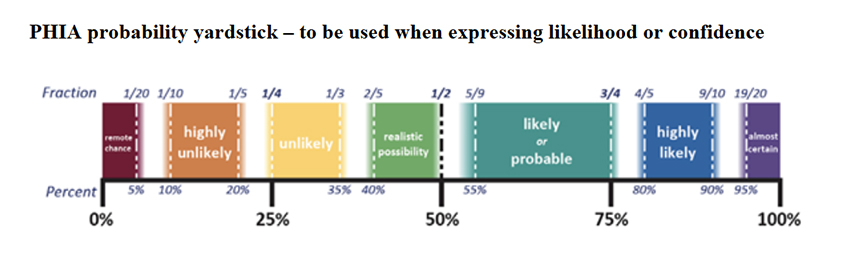 It means a 50-50 situation, a coin flip. While there is a reason for concern, you need to keep in mind that
It means a 50-50 situation, a coin flip. While there is a reason for concern, you need to keep in mind that
- B.1.1.7’s fatality rate is low 0.09%, it is the relative risk that appears to be so much more significant, and that is the number being tossed about.
- Only time and a more extensive collection of patients with reliable data will answer whether it is more lethal.
- The current data is based on a small sample with variations in measurements.
When taken together, we simply do not know whether it is or isn’t going to be a bigger problem.
Source: NERVTAG note on B.1.1.7 severity New and Emerging Respiratory Virus Threats Advisory Group