Before jumping in, let me share one definition you may not be familiar with, dual eligibility. These are patients receiving both Medicare and Medicaid; Medicare because of their age, disabilities, or end-stage renal disease, Medicaid because their incomes are at or below the established federal poverty level ($12,800 annually). They tend to be “sicker, more depressed, and reporting more pain than Medicare-only beneficiaries.”
Dual eligibility represents about 20% of the Medicare beneficiaries, but 66% of those in nursing homes. The greater percentages are partly because nursing-home care is expensive and that once the cost of their care has absorbed beneficiaries' assets, they fall below the federal poverty guidelines and become dually eligible.
Nursing Home Utilization and COVID-19
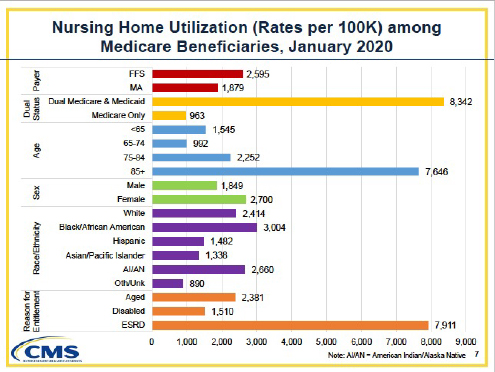
The graphic breaks down all Medicare beneficiaries in 2020 – given as beneficiaries per 100,000 adjusts for differences in demographics. Blacks and Indigenous Americans were 20% and 10% more likely than White beneficiaries to be in nursing homes; Hispanics and Asian Americans were 39% and 45% less.
The data is based on billing codes. 22% of reported COVID-19 cases were nursing home residents; they were 14 times more likely to be diagnosed with COVID-19 than Medicare beneficiaries living in the community. Even when community levels of COVID-19 were low, nursing home cases were 11-fold more likely to be diagnosed with COVID-19. In looking at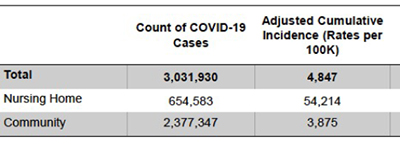 beneficiaries' demographics, i.e., age and ethnicity, the most impactful cause for a diagnosis of COVID-19 was institutional status – living in a nursing home. Imperfectly reflecting community rates, blacks were 11% more likely, Hispanics 19% more likely, and Asians 7% more likely to be diagnosed with COVID-19 than their White nursing home counterparts. Indigenous Americans were 4% less likely to carry this diagnosis.
beneficiaries' demographics, i.e., age and ethnicity, the most impactful cause for a diagnosis of COVID-19 was institutional status – living in a nursing home. Imperfectly reflecting community rates, blacks were 11% more likely, Hispanics 19% more likely, and Asians 7% more likely to be diagnosed with COVID-19 than their White nursing home counterparts. Indigenous Americans were 4% less likely to carry this diagnosis.
Hospitalization and Death
As might be expected by case volume and the inherent frailty of nursing home patients, they were hospitalized more than community-dwelling beneficiaries – 12 times more likely, that 2% of beneficiaries accounting for 19% of hospitalizations. All ethnicities, Black, Hispanic, Asian, and Indigenous Americans, were more likely to be hospitalized; 70%, 64%, 60%, and 21%, respectively.
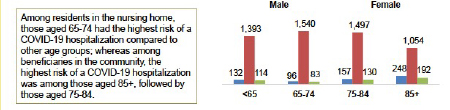 When stratified by age, there was a distinct difference. Those age 65-75 in nursing homes had the highest risk of hospitalization; for community-dwelling beneficiaries, the age group was 85+.
When stratified by age, there was a distinct difference. Those age 65-75 in nursing homes had the highest risk of hospitalization; for community-dwelling beneficiaries, the age group was 85+.
Chronologic age is a poor measure of frailty. Assuming for a moment that a correspondence can be suggested, nursing home patients, because of their underlying co-morbidities, are 10 to 20 years “older,” physiologically, than their community-dwelling compatriots. As you might expect, the great driver of hospitalization was again institutionalization – living in a nursing home.
This chart breaks out the underlying chronic conditions followed by CMS. From the visualization, it should be 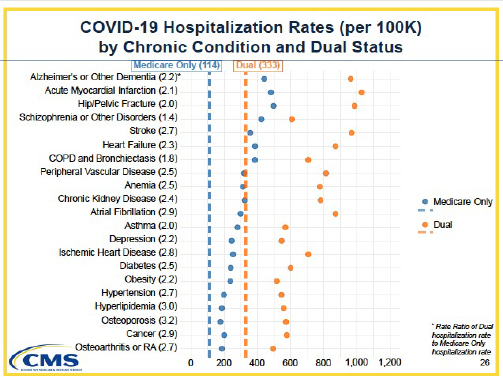 apparent that the dual eligible have a higher incidence of co-morbidities; no surprise, that is why they are in nursing homes. But the chronic conditions that resulted in hospitalization are those that more frequently require more than a daily medication. Alzheimer's, Hip and pelvic fractures, stroke all require care to assist with the activities of daily living (ADLs) – getting dressed, bathed, eating. That requires more interaction with the staff. Staff that currently is only 60% vaccinated.
apparent that the dual eligible have a higher incidence of co-morbidities; no surprise, that is why they are in nursing homes. But the chronic conditions that resulted in hospitalization are those that more frequently require more than a daily medication. Alzheimer's, Hip and pelvic fractures, stroke all require care to assist with the activities of daily living (ADLs) – getting dressed, bathed, eating. That requires more interaction with the staff. Staff that currently is only 60% vaccinated.
Finally, again as we might suspect, far more nursing home patients died from COVID-19 than those in the community, 43% versus 22%. Institutionalization was again the one factor with the most significant impact. More importantly, CMS found no clear association between co-morbidities and institutional status to explain the higher mortality. I interpret that to mean that co-morbidities resulted in similar events irrespective of whether the beneficiary was living in the community or nursing home.
If it is not co-morbidities and the care they require in the institutions, we are left with environmental exposure within the nursing homes. What is different between nursing homes and community living – our comings and goings. In nursing homes, the most significant source of variation in environmental exposure is the coming and going of the staff.
CMS does have data on vaccinations by nursing home personnel. That is the source of that 60%, actually 61.1%, figure mentioned previously. But, the aggregate covers some significant disparities. Now, I would like to caution that the data set used to determine these numbers is a bit fuzzy; it indicates that over 200% of physicians have been vaccinated – apply as many grains of salt as you like to the following table, based on data current on August 15th.
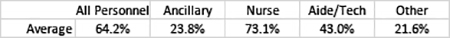 Look at the vaccination rates for the nurses, which is roughly what is being reported in other health care settings. Now consider the rates of vaccination for aides and techs – the people that provide the actual face-to-face care, the personnel who have the greatest exposure to the patients. Those other groups, including transport, housekeeping, dietary services, have even lower vaccination rates, but their direct contact may be more limited.
Look at the vaccination rates for the nurses, which is roughly what is being reported in other health care settings. Now consider the rates of vaccination for aides and techs – the people that provide the actual face-to-face care, the personnel who have the greatest exposure to the patients. Those other groups, including transport, housekeeping, dietary services, have even lower vaccination rates, but their direct contact may be more limited.
These vital members of the healthcare team are, to my mind, doing harm, needlessly exposing vulnerable patients because of their “rights or hesitancy.” These unexpectedly low vaccination rates explain the decision by President Biden to require all nursing home staff to be vaccinated as a condition of participating in the Medicare and Medicaid programs.
Source: The Impact of COVID-19 on Medicare Beneficiaries in Nursing Homes




