The United States is in the throes of a surge of serious infections with the COVID-19 Delta variant. The seven-day average of COVID-19 new admissions to hospitals nationwide has exceeded 11,000 for the past few weeks, overwhelming healthcare capacity in several states.
The situation is worst in ICUs, which care for the sickest patients with highly specialized medical staff who are in short supply and are becoming progressively burned out as the pandemic drags on. The result is that in many parts of the country, patients needing to be hospitalized are being shuttled long distances to available beds and are receiving substandard care due to staffing shortages.
Given the abundance of readily available, free, effective (albeit imperfect) vaccines for many months, what is going on? There are three primary factors at work that dictate the severity of an outbreak of a viral illness.
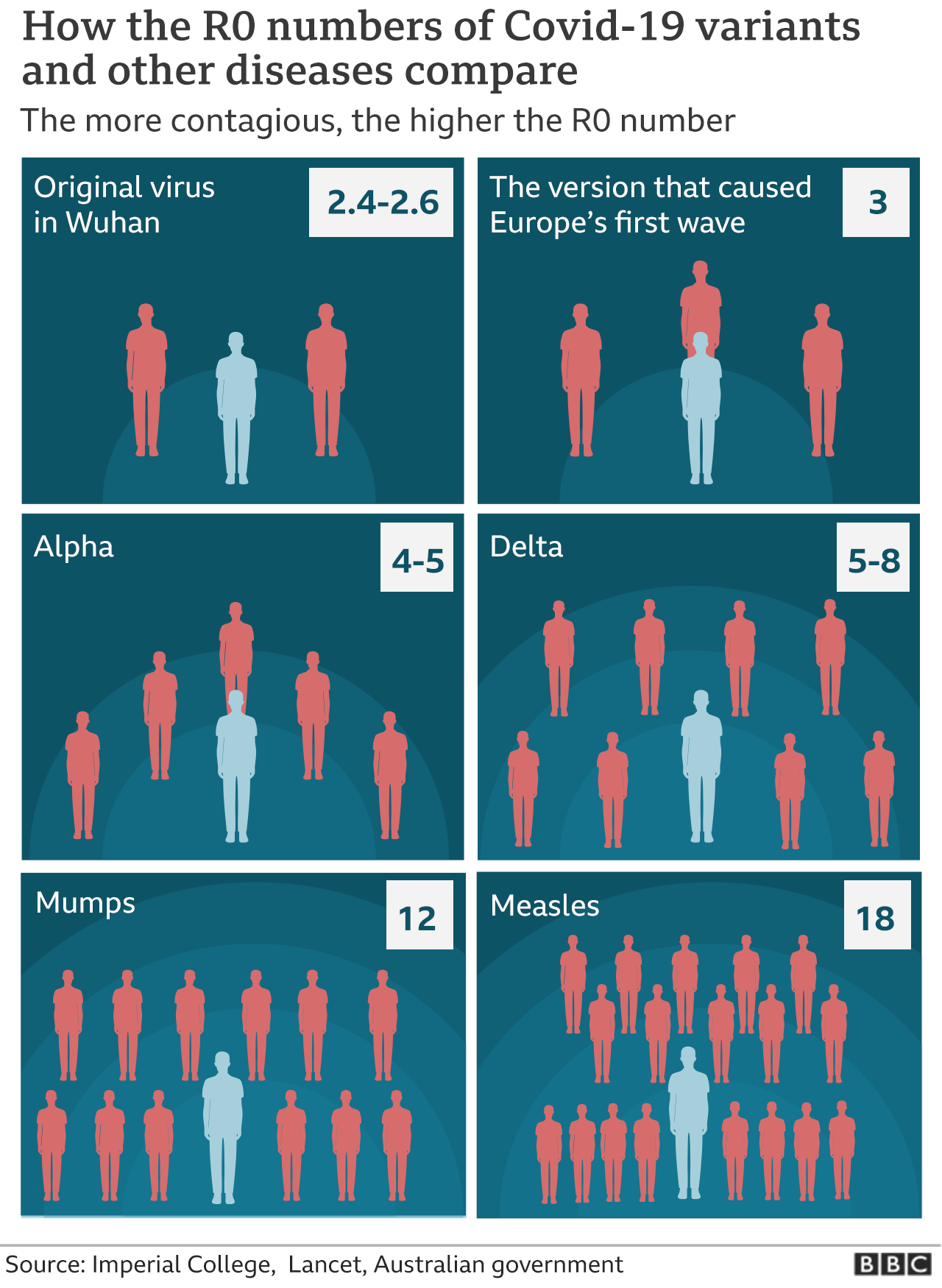
The first is the profile of the virus, which itself has two variables – transmissibility, or infectiousness; and virulence, the severity of illness in people who become infected. The first of these is represented by a variable called R0, or R-naught. As illustrated in the figure below, the Delta variant of the SARS-CoV-2 virus, which causes COVID-19, and which is now dominant in the United States, is more than twice as infectious as the original Wuhan coronavirus, and about half again as infectious as the once-dominant Alpha variant.
That is important, because it means that once relatively safe activities and casual contacts now have a higher probability of transmitting infection. That means that our perceptions of the risk of various activities may need to be modified. In July 2020, the Texas Medical Association published a helpful table (below) of the comparative risk of various activities during the pandemic. Given the characteristics of the Delta variant of SARS-CoV-2, we might need to bump up the risk level of some of those activities, especially ones that involve close contact with other people in indoor settings. So, for example, attending a wedding or funeral, shown in the table as “Moderate-High Risk,” might now be more appropriately considered to be “High Risk,” especially if people are densely packed and the ventilation isn’t good.
As to virulence, a large, recently published British study found “a higher hospital admission or emergency care attendance risk for patients with COVID-19 infected with the delta variant compared with the alpha variant.”
Thus, with Delta we have a virus that is both more transmissible and more virulent. Not surprisingly, then, outbreaks, especially in populations with low vaccination rates, are a much greater burden on healthcare systems than the earlier variants. Moreover, every COVID-19 infection involves the replication of the virus’ RNA, which gives rise to more mutations and new opportunities for even more-worrisome variants to emerge.
The second factor that determines the severity of an outbreak is the state of immunity of potential hosts, or victims, of the virus. The first line of defense is the “innate immune response,” which consists of nonspecific physical, chemical and cellular defenses against pathogens. The second line of defense is the adaptive, or acquired, immune response, which is mediated by white blood cells called lymphocytes, in response to a pathogen or to a vaccine that protects against that pathogen. Some lymphocytes produce specific anti-pathogen proteins called antibodies, while others attack the pathogen directly.
Only about 60% of the U.S. population is fully vaccinated, and on July 28, a study published as a preprint (that is, not yet peer-reviewed) showed that the Pfizer-BioNTech vaccine’s efficacy against symptomatic disease had slipped from 96% to 84% after six months. Such findings are spurring discussions about when vaccine booster doses will be needed, and to whom they’ll be offered.
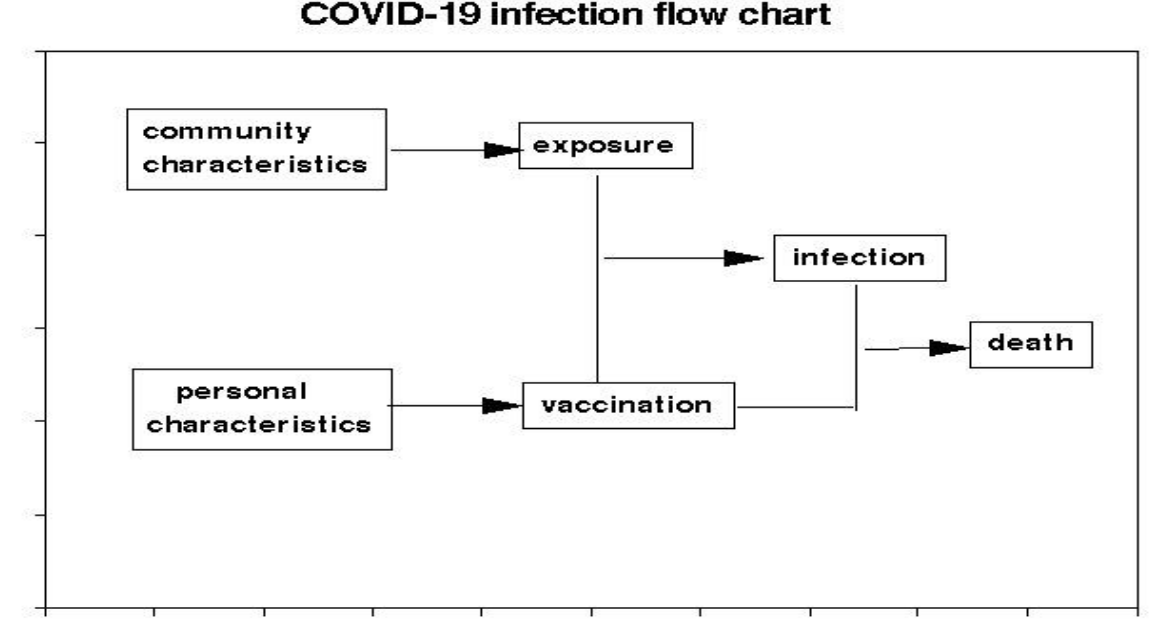
The third factor affecting outbreaks is the behavior of individuals and policy makers. Vaccination, whether voluntary or mandated, is our most potent weapon to suppress symptomatic infections and, thereby, “flatten the curves” of hospitalizations and deaths. “Non-pharmaceutical interventions” (NPIs), such as masks, social distancing, avoidance of crowded indoor spaces, and good ventilation are also effective. As illustrated by this figure, first conceived by Australian virologist Ian Mackay, the more NPIs (in conjunction with vaccines), the better:
A July incident in Marin County, California – one of the nation’s most-vaccinated locales -- illustrates what can happen when people behave irresponsibly. During May 23–June 12, 26 laboratory-confirmed COVID-19 cases occurred in elementary school students and their contacts following exposure to an unvaccinated, infected, symptomatic teacher who removed her mask to talk to the students. The infection rate in one affected classroom was 50%, and the risk of infection correlated with students’ seating proximity to the teacher.
In Illinois in June, a church sponsored a five-day teen camp and a two-day men's retreat. Masks and vaccines weren't required, and those events were linked to at least 180 COVID-19 infections, according to the CDC.
Another example occurred in South Dakota, where COVID-19 cases spiked following the August Sturgis Motorcycle Rally, when hundreds of thousands of bikers descended upon the area. Between August 4, the date closest to the start of the rally for which data were available, and August 25 (ten days following the end of the rally), the state reported an increase in active COVID-19 cases of 456%.
Policymakers must carefully balance questions of citizens’ freedom of movement and actions with public health considerations. Permitting superspreader events and the banning of mask or vaccination mandates clearly impede control of the pandemic and prolong the misery and the proliferation of cases, hospitalizations, and deaths.
We have the tools to flatten the curve, and if we are to reach some sort of modus vivendi with the SARS-CoV-2 virus, we need to use them.
Note: An abbreviated version of this article appeared in the Washington Examiner.




