All sensation goes through four stages or processes; let’s go through them in turn.
Transduction
Unlike localized, aggregated receptors of the eye (retina), ear (nerve endings of the cochlear nerve found in the middle ear), or tongue (taste buds), pain receptors, nociceptive nerve endings, are scattered throughout our body. They are like the proprioceptive receptors of touch and position. They respond to heat, mechanical deformation, and chemicals, often found in inflamed areas. The majority of studies involve pain receptors in the skin where we can create burns, cuts, or inflammation. The majority of our clinically significant pain is musculoskeletal or visceral (from our organs), and those studies are few and far between if they are to be found.
Transmission
The signal from the pain receptors, written like Morse code, as a pattern and frequency, travels from these peripheral sites to the more central spinal cord. At this point, the signal splits into two. One signal, remaining “local,” initiates a withdrawal reflex, a behavior. Burn your finger, and you withdraw your hand from the heat source. A second signal is sent upwards into areas within our brain. The two major sites are the thalamus and medial reticular formation of the brain stem. We will not be pursuing how those signals move about the brain; it is sufficient to know that further processing of those signals, and ultimately “detection and identification” of our perception of pain, occurs here.
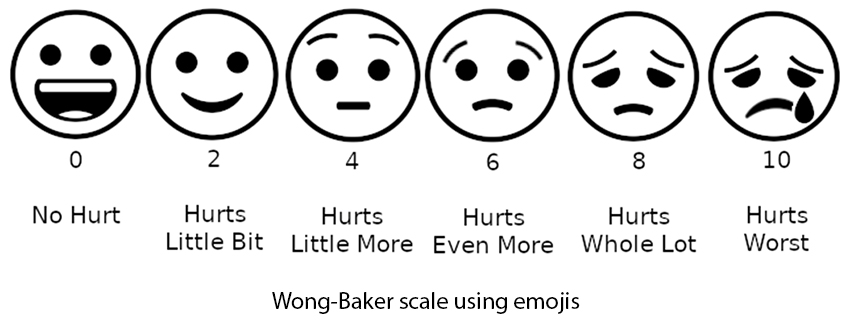
This split of the signal means that most of our animal studies focus on pain identified as a behavior that reflex to noxious stimuli. But we have no accurate means of quantifying the signal traveling into the brain, no real way of measuring the experience of pain – we must always speak in necessarily fuzzy terms, be it emojis or numbers, including morphine milligram equivalents.
 Our other senses also create these split signals. For example, the visual receptors in the retina send a signal inward to convert that information about light and color into an “image.” Meanwhile, like the withdrawal reflex, behavioral reflexes respond to those retinal signals. The vestibulo-ocular reflex coordinates the position of your head with the incoming visual information keeping your image of the world stable despite the movement of your head and eyes.
Our other senses also create these split signals. For example, the visual receptors in the retina send a signal inward to convert that information about light and color into an “image.” Meanwhile, like the withdrawal reflex, behavioral reflexes respond to those retinal signals. The vestibulo-ocular reflex coordinates the position of your head with the incoming visual information keeping your image of the world stable despite the movement of your head and eyes.
Our senses also elicit an additional emotional (affective) response, our likes and dislikes regarding art, music, or food. Pain, on the other hand, is unidirectional; we want less of it and want it to go away. Pain’s emotional component acts more like a deep “drive,” say hunger, resulting in actions to terminate the noxious stimulus. When we hear music we do not like or a displeasing picture; we do not experience the same emotional, “visceral,” response. This is a crucial distinction between pain from our other senses
The biological duality between the sensory reflex of withdrawal and the more centrally formed emotional response makes measuring pain difficult. In a laboratory setting, we can define a sensory threshold for pain reception, the reflex; heating the skin between 43-46º C will elicit a pain response. But the “tolerance” of pain, the affective, emotional component, can vary widely.
“The tolerance for pain is a complex function that may be modified by personality traits, attitudes, previous experience, economic factors, gender, and the particular circumstance under which the pain is experienced.”
Modulation
As with all senses, our nervous system can up and down-regulate our affective experience of pain.
Consider that perennial summer favorite, the sunburn. The normally warm water of your evening shower on that sunburn is now suddenly more painful – you are more sensitized to the experience of pain. When overly active, our sympathetic nervous system, our fight or flight system, causes us to experience a greater degree of pain. Makes sense that when we are already in a heightened state of fear, noxious stimuli will get additional attention and response.
Anxiety and stress are common reasons for sympathetic nervous system arousal. To some degree, this can create a self-fulfilling cycle; fear of pain increases our perception of pain, which in turn increases our fear. This may well explain the therapeutic benefits of adjunctive pain relief, like music, which reduces the sympathetic tone and down-regulates our “experience” of pain.
Neural pathways rather than pain receptors can also produce pain. Perhaps the most common example would be the pain after an episode of shingles – a late result of having had chickenpox. While the acute pain of this often debilitating “rash” is due to the pain receptors in your skin, the chronic pain, which can last for months, is not. Post-herpetic neuralgia, its medical name, is a longer-term (up to six months or more in those over age 60) inflammation of the nerve pathways that can result in continued chronic pain long after the skin rash has disappeared.
Perception
These three processes, transduction, transmission, and modulation, come together to form our perceptional experience of pain. Because our perception of pain requires all three of these biological processes, all of which may differ from one individual to another. For a given painful stimulus, my experience of pain may well differ from yours, and my experience of that painful stimuli may vary over time.
When the rubber hits the road, “What we have here is a failure to communicate.”
We can listen to music, view the sunset, or experience a rough surface and have some basis to share and communicate those experiences. Pain, unlike those other senses, remains subjective; it is your experience, not mine. One of the great difficulties we have in medical care is finding a way to communicate our experience of pain. Unlike temperature or blood pressure, there is no convenient instrument or numerical value to quantify pain. Without the ability to quantify pain or at least place it on some shared scale, physicians are without guidance on treating pain effectively. In the not-so-distant past, to fill that communication void, physicians would substitute their “experience” of pain for the ambiguous description by the patient; or, more commonly, would follow the “rule of thumb” prescription taught to them by the intern or resident. [1]
Much of the consternation in the “community” of patients with chronic pain results from our biological inability to readily share our experience of pain. Patients are often left with rigid guidelines, a one-size-fits-all approach that clearly is incompatible with our understanding of pain’s biology. Or left with a physician, substituting their experience, training, and subjective beliefs about addiction, malingering, doing no harm, and serving the best interests of their patients, in prescribing treatment. That is why pain is both under and overtreated; despite all our scientific knowledge, the experience of pain remains a black box. We are all blind men seeking to describe the elephant.
What we have here is a failure to communicate. It needn’t be the case, but getting “into the mind” of another is more difficult than we might think, especially in a healthcare system driven by the clock. Need proof? Look at how vehement the opposing views on any public concern where there is objective data we can all see, hear and touch
[1] Like an entire generation of physicians, I was taught that the routine treatment for post-operative pain was Demerol 75mg and Vistaril 50mg given every 3 to 4 hours by intramuscular injection. I learned this from my intern when I was a fourth-year medical student writing orders.
Sources: The Anatomy and Physiology of Pain National Library of Medicine