The global study involved data and scientists from the Multi-Country Multi-City (MCC) Collaborative Research Network. The dataset, daily ambient temperatures, relative humidity, and pollutants (PM10, PM2.5, ozone, and NO2) across 567 cities in 27 countries.
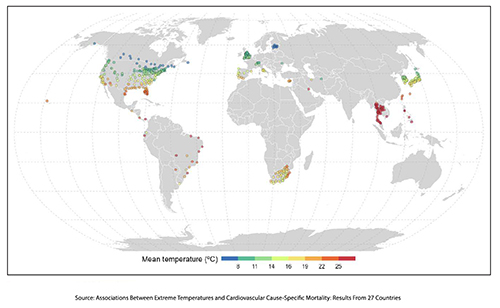 As you can see from this mapping of mean temperatures, the data come predominantly from just a few global spots, and visually, colder climes seemed more represented. [1]
As you can see from this mapping of mean temperatures, the data come predominantly from just a few global spots, and visually, colder climes seemed more represented. [1]
The cardiovascular outcomes of concern, deaths from ischemic heart disease (heart attacks), strokes, heart failure, and arrhythmias (abnormal heart rhythms. Over a forty-year period, they identified 32 million plus cardiovascular events
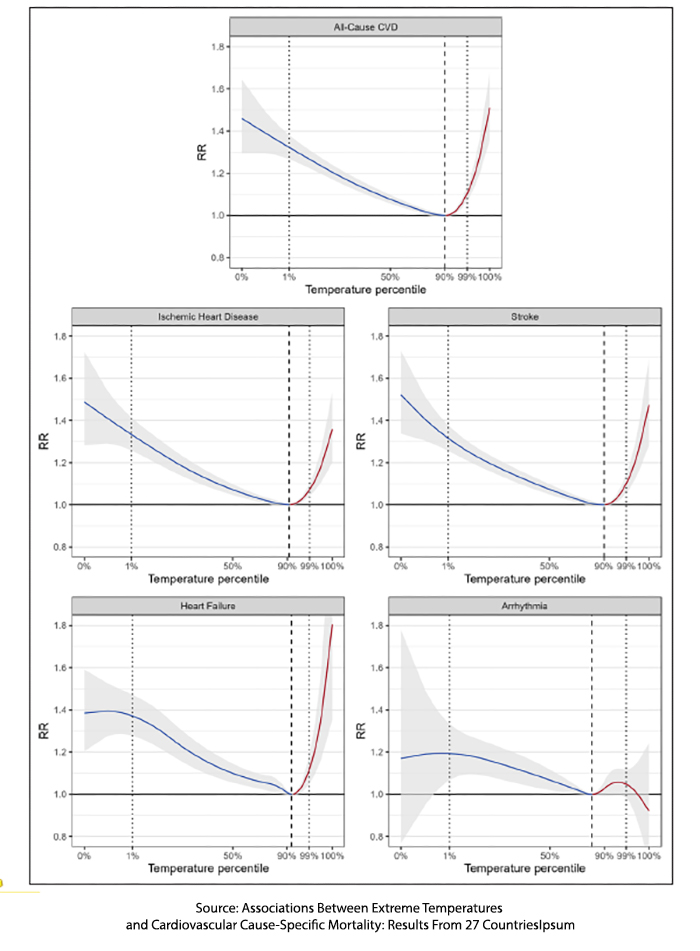
- Except for the deaths from arrhythmias, all the cardiovascular deaths have the general shape of that Goldilocks, Nike swoop – excess deaths at the extremes and a range of temperatures more conducive to our health.
- Cold temperatures resulted in more excessive deaths than heat, 9.1 per 1000 deaths versus 2.2 per 1000 deaths. For those who like their ratios as percentages, cold deaths contributed 0.91% and heat deaths 0.22% to excess deaths – a small effect.
- Based upon the slope of the data, rising heat resulted in deaths over a shorter number of days; cold deaths were both greater and over a longer time frame.
- In both instances, deaths from heart failure were more significant than the other cardiovascular outcomes.
- Arrhythmias were a bit of an outlier. There were far fewer to evaluate, with a far lower effect; in the words of the researchers, “risk of dying from arrhythmias was associated with greater uncertainty.”
- In a sensitivity analysis, looking for whether a variable had a more pronounced impact on their results, the researchers found that increases in the lag time between a temperature event and death slightly increase the cold deaths.
- And then there was this contrarian statement, going against many of the publications on other environmental factors influencing excess mortality.
“The results were unaffected by adjustments for temperature variability, heatwaves, long-term trends, relative humidity, and air pollutants (e.g., ozone, nitrogen dioxide, particulate matter [PM10, and PM2.5]" Emphasis added
Another factor that decreased these temperature-related deaths was increasing GDP, a measure of a country’s wealth. The researchers wondered whether wealthier countries could mitigate temperature with heating and cooling systems and that they might feature less outdoor work where individuals were more exposed to ambient temperature.
A Physiologic Basis?
The Goldilocks range I alluded to earlier reflects the autonomic and cardiovascular changes we have to temperature, ensuring an optimal internal temperature for our metabolism – neither too hot nor too cold. These normal responses alter with aging and can be further perturbed by disease of our cardiovascular system, which is one of the great engines of heating and cooling.
We shed heat by increasing blood flow to our skin, radiating heat away, and by increased sweating, which cools by evaporation. Our evaporative losses can be significant and sufficient to reduce the overall volume of fluid being moved by the heart. Under these circumstances of volume loss, our heart compensates by increasing its rate of beating and contractility – moving as much blood as we need despite the lower overall volumes. This increases the work of the heart and its need for oxygen; increasing internal temperature also increases our metabolic rate, another cause of increased oxygen consumption. For those with coronary artery disease, that may be sufficient to tip the balance into dis-ease. Those volume changes are also buffered by fluid within our cells, which can lead to electrolyte balance alterations – a source of arrhythmias. That volume loss also increases blood concentration and makes us more susceptible to forming clots, heightening the risk of heart attacks.
To maintain warmth, we close the blood flow to our skin, moving more warm blood inwards. We increase muscle tone and begin to shiver, which generates heat but also increases our blood pressure. Increasing blood pressure puts more work on the heart, increasing the need for oxygen when coronary artery disease may limit how much more oxygen can be provided – leading once again to heart attacks. As with our attempts to control heat, our bodily fluids shift, decreasing our blood volume not by evaporation from sweating but by movement into cells. Once again, that concentration of the blood can heighten the risk of clotting, heart attacks, and strokes.
“The results illustrate the relevance of environmental exposures to specific CVD causes of mortality and have direct relevance to prompt optimal medical and public health responses to temperature extremes in present day and under a changing climate.”
What might those responses be? For all the data collection flaws, the study speaks to an old scientific principle, survival of the fittest. In a changing environment, those with cardiovascular disease seem to do poorer. Those excess deaths from temperature reflect the frail and fragile who live much longer today because of better medical treatment; parenthetically part of why there are fewer deaths in countries with higher GDP. I will leave the optimal public health strategies to others; we just need to eat a sensible diet, exercise, and not smoke, the three risk factors we can all modify.
[1] This geographical predominance of some data illustrates the old story of the drunk looking for his keys under the streetlight. The data reflects areas that can provide daily meteorologic data and health statistics.
Source: Associations Between Extreme Temperatures and Cardiovascular Cause-Specific Mortality: Results From 27 Countries Circulation DOI: 10.1161/CIRCULATIONAHA.122.061832