Despite the scare tactics of “Reefer Madness” and Harry Anslinger, the “OG” warrior of the federal Bureau of Narcotics, cannabis in the 60s and 70s was not considered a “drug of dependence,” primarily because there was no documentation of tolerance or withdrawal symptoms. Over time, the American Psychiatric Association, the group responsible for the DSM, changed its definition of addiction, describing “substance use disorder,” emphasizing the behavioral rather than physiologic signs and symptoms.
“The essential feature of Substance Dependence is a cluster of cognitive, behavioral and physiologic symptoms indicating that the individual continues use of the substance despite significant substance-related problems.”
Estimates of the number of cannabis-dependent individuals widely vary, although it is generally accepted that longer use fosters dependence. One study of our national comorbidities in the mid-1990s suggested that 9% of cannabis users evidenced substance dependence at some time in their lives. For context, substance use disorder was present at some time for 32% of nicotine users, 23% of heroin users, and 15% of users of alcohol.
The diagnosis is based upon a patient meeting two or more criteria. [1] Studies have demonstrated tolerance to cannabis, most likely secondary to physiologic changes in the function of cannabinoid receptors. Additionally, there appears to be a pattern of withdrawal symptoms, including “anxiety, insomnia, appetite disturbance, and depression.” Leaving aside the changes in appetite, the other three symptoms raise another question, especially when considering the medicinal use, physician or self-prescribed, of marijuana.
Which came first, the anxiety, insomnia or depression, or the use of marijuana?
That question lies at the heart of a recent viewpoint on cannabis use disorder (CUD) in JAMA Psychiatry. Simply put, are the current DSM criteria for substance use disorder appropriate when considering cannabis use as therapeutic rather than recreational?
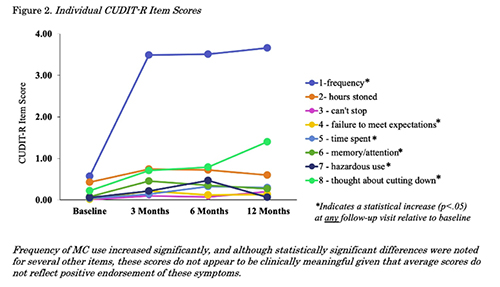 A study looked at 54 patients, all “cannabis-naïve,” being medically treated with cannabis for various disorders, including pain, anxiety, mood, or sleep-related symptoms. A self-reported questionnaire was completed at the initiation of therapy and 3-month intervals over a year. The survey, entitled CUDIT-R, includes eight items and has been validated among recreational users to assess substance dependence. [2]
A study looked at 54 patients, all “cannabis-naïve,” being medically treated with cannabis for various disorders, including pain, anxiety, mood, or sleep-related symptoms. A self-reported questionnaire was completed at the initiation of therapy and 3-month intervals over a year. The survey, entitled CUDIT-R, includes eight items and has been validated among recreational users to assess substance dependence. [2]
As the chart indicates, the primary finding was an increased frequency of use during that initial 3-month period. The researchers concluded that CUDIT-R was a poor measure of possible cannabis use disorder among patients using marijuana for medical purposes.
When cannabis is used therapeutically, it would not be uncommon to change dosages, especially during the initial treatment period. And if the treatment is effective, it would be anticipated that cessation of the drug would result in withdrawal symptoms. But the mere presence of these symptoms, irrespective of the reason, is sufficient to diagnose cannabis use disorder, at least as the DSM criteria are now written. While the DSM cautions that tolerance and withdrawal “should not be the primary basis for diagnosing CUD in a therapeutic setting,” that may not be the guidance followed by today’s contemporary Harry Anslingers or Physicians for Responsible Opioid Prescribing (PROP).
The current JAMA viewpoint argues that cannabis use disorder requires a different definition when used therapeutically rather than recreationally. That
“explicitly acknowledging expected neuroadaptation in the context of cannabis use to address a chronic physical or psychological problem[s]”
would bring it in line with the DSM's cautions on prescription medication misuse. Of course, if you speak with pain patients, you will find that misuse of the DSM criteria for substance dependence is pandemic.
Could it be that opioid use disorder conflates therapeutic and recreational use, something that pain patients have been claiming for years? Does that account for their determination that 8-12% of those receiving opioids have a substance use disorder? I agree with the authors, therapeutic uses of drugs under physician supervision, be they opioids or marijuana, are not necessarily “addictive” based solely on the changing dosage and presence of withdrawal symptoms. Applying the current DSM criteria in a therapeutic setting makes little sense and needlessly labels patients as having a substance use disorder – the damage to patients with chronic pain using opioids is already well established.
[1] The DSM-5 defines Substance Use Disorder as a problematic pattern of substance use leading to significant impairment or distress, as manifested by at least two of the following criteria occurring within a 12-month period:
1. Substance is often taken in larger amounts or over a longer period than was intended.
2. Persistent desire or unsuccessful efforts to cut down or control substance use.
3. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from its effects.
4. Craving, or a strong desire or urge to use the substance.
5. Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home.
6. Continued substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the substance.
7. Important social, occupational, or recreational activities are given up or reduced because of substance use.
8. Recurrent substance use in situations in which it is physically hazardous.
9. Substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance.
10. Tolerance, as defined by either of the following:
- A need for markedly increased amounts of the substance to achieve intoxication or desired effect.
- Markedly diminished effect with continued use of the same amount of the substance.
11. Withdrawal, as manifested by either of the following:
- The characteristic withdrawal syndrome for the substance.
- The same (or a closely related) substance is taken to relieve or avoid withdrawal symptoms.
Footnote courtesy of ChatGPT
[2] “hours stoned during days of use; inability to stop using once started; failure to meet expectations; time spent getting, using, or recovering from cannabis; memory or concentration problems after cannabis use; using in hazardous situations (e.g., driving, caring for children); and desire to stop/reduce cannabis use.”
Sources: Cannabis Use Disorder (CUD) in the Context of Cannabis for Therapeutic Purposes (CTP) JAMA Psychiatry DOI: 10.1001/jamapsychiatry.2023.0053
Assessing Cannabis Use Disorder in Medical Cannabis Patients: Interim Analyses from an Observational, Longitudinal Study Cannabis DOI: 10.26828/cannabis/2021.02.
The Health and Psychological Effects of Cannabis Use National Drug and Alcohol Research Center University of South Wales




