“Cannabis is among the most frequently used psychoactive substances in the world,” a fact undoubtedly true. A Gallop poll puts U.S. use at 16% of the population. For context, 12.5% of Americans smoke tobacco, and 63% of us drink alcohol.
This ain’t your Daddy’s weed.
Unlike the other two drugs, the concentration of the main psychoactive component of cannabis, THC, has steadily increased since the 60s, rising from 10% in 2009 to 14% in 2019. There has also been a rise in cannabis use disorder (CUD) from 4.9% to 5.9% among the most active smokers, 18 to 25-year-olds - who also happen to be the age group at the most significant risk for the clinical onset of schizophrenia. These three facts, these dots, beckon to the researchers to be neatly tied together.
“The increased THC content may thus, along with a potential increase in the prevalence of CUD, be a main driver of the population-level increase in PARF [population attributable risk fraction] between CUD and schizophrenia.” [1]
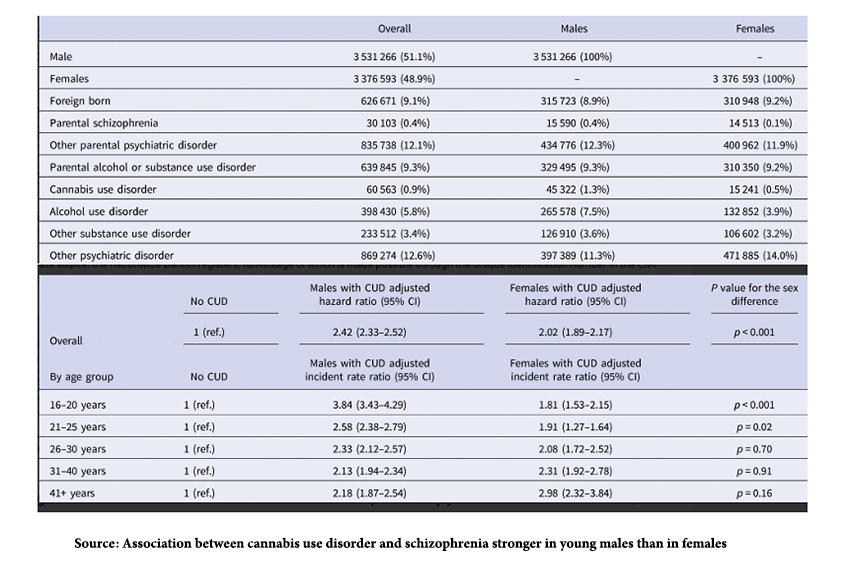
To connect the dots, they used nationwide Danish registries on psychiatric disorders for all patients aged 16 to 49 between 1972 and 2021. Those registries recorded all inpatient treatments since 1969; all outpatient treatments were added in 1995 – so we have a comprehensive data set. Here is a portion of their data on the demographics and findings in the dataset of individuals diagnosed with CUD and schizophrenia.
- A genetic or heritable component is present, 0.4% for parental schizophrenia, but 12% for all parental psychiatric disorders. There is also a significant component of parent alcohol or substance use disorders at 9%.
- Cannabis is not the only abused substance. Alcohol abuse is roughly five-fold more frequently reported.
- Other psychiatric problems co-exist. In fact, the presence of other psychiatric diseases was a stronger factor; in “adjusting,” for the presence of other psychiatric disorders, the final hazard risk of cannabis, was reduced almost10-fold. The researchers write, “… some of these other psychiatric disorders might well be intermediate diagnoses between CUD and schizophrenia, and thus act as mediators rather than confounders.”
- Males were impacted more than females. As a generalization, there appears to be a somewhat greater prevalence of schizophrenia in males, and it presents earlier than in females – two findings consistent with the CUD hazard ratios reported.
These dots in the narrative are all factual, but the researchers make a leap of faith in connecting those data points.
“Assuming causality, approximately 15% of recent cases of schizophrenia among males in 2021 would have been prevented in the absence of CUD; by contrast, among females, 4% of recent cases of schizophrenia would have been prevented if they did not have CUD. …
At the population level, this translates to CUD being a major modifiable risk factor for schizophrenia, particularly among males. Notably, an increasing proportion of cases with schizophrenia may be avertible by preventing CUD, and this increase is likely linked to the increase in THC concentration in cannabis…” [emphasis in bold added]
I am not ready to make that leap. There is more science to consider. I am willing to consider cannabis, and for that matter, alcohol gateways to mental disease, but I believe it may be more critical to recognize that the gate swings both ways – that is, schizophrenia, in this instance, is a gateway to substance abuse. Interestingly, the same investigator in this study, using the same albeit a bit older Danish registry, has written that:
“A diagnosis of schizophrenia was positively associated with the risk of developing substance abuse … primarily associated with an increased risk of abuse of cannabis, alcohol, stimulants and other substances”[2]
The narrative can go in either direction. There is one more study to mention that looks at 232 patients being initially diagnosed with schizophrenia.
“Alcohol abuse prior to first admission was found in 24%, drug abuse in 14%—twice the rates in the general population. Alcohol abuse more often followed than preceded the first symptom of schizophrenia. Drug abuse preceded the first symptom in 27.5%, followed it in 37.9%, and emerged within the same month in 34.6% of the cases. The study demonstrates a remarkable association between first-episode schizophrenia and substance abuse, but a unidirectional causality is not supported, nor is a specific psychotic disorder in comorbid cases.”
Can cannabis be a trigger? Yes. Is it a modifiable risk factor? Perhaps. Is 15% of schizophrenia due to cannabis use disorder, as the Danish study assumes? Not likely.
Here is the bonus for those who have read so far. This which-came-first dilemma of substance abuse and mental illness was made dramatically clear to me during a visit to Key West and the home of Ernest Hemingway. Hemingway was one of our greatest writers. Hemingway was an amateur boxer and survived two plane collisions – he had some degree of physical injury to his brain, concussions at the very least. Hemingway, by most measures, suffered from alcoholism which we would now term alcohol use disorder. Mental illness was a significant family problem. “Seven of Hemingway’s close family relations died by suicide, including his father, sister, brother and much later his granddaughter, the supermodel Margaux Hemingway.” Hemingway captures the bidirectional gate that is mental illness and substance abuse. [3]
[1] As a reminder, the Population Attributable Risk Fraction (PARF) represents the fraction of total disease in the population that is attributable to a risk factor. You can read a bit more about PARF here.
[2] For those who must know, the Hazard ratio for schizophrenia and substance abuse was 3.64, 2.48 for cannabis specifically, and 1.95 for alcohol.
[3] Hemingway’s medical history, especially his ECT treatments at Mayo Clinic, adds much context to his life and final years. You can read more here.
Sources: Association between cannabis use disorder and schizophrenia stronger in young males than in females Psychological Medicine DOI: 10.1017/S0033291723000880
Schizophrenia is associated with increased risk of subsequent substance abuse diagnosis: A nationwide population-based register study Addiction DOI: 10.1111/add.14746
Substance Abuse and the Onset of Schizophrenia Biological Psychiatry DOI: 10.1016/S0006-3223(95)00609-5
How mental health struggles wrote Ernest Hemingway’s final chapter PBS News Hour