Infants and toddlers, as any parent or grandparent can attest, are vectors of disease. In the case of COVID, metaphorically, they may be more like enzymes, catalyzing infections for those around them but unaffected by the virus itself. Seroprevalence studies suggest that well over 96% of the little ones have COVID antibodies
The study, reported in Cell, looked at systemic immunity utilizing blood samples from 54 infants and young children (2 weeks to 47 months old) infected with various strains of COVID, as well as 27 infants with paired pre-infection samples. Paired samples were collected before, during, and after infection. Additional blood samples were taken from adults with and without COVID as well as 41 mothers with “mild” COVID – median age 59. Mucosal immunity was measured with weekly nasal swabs.
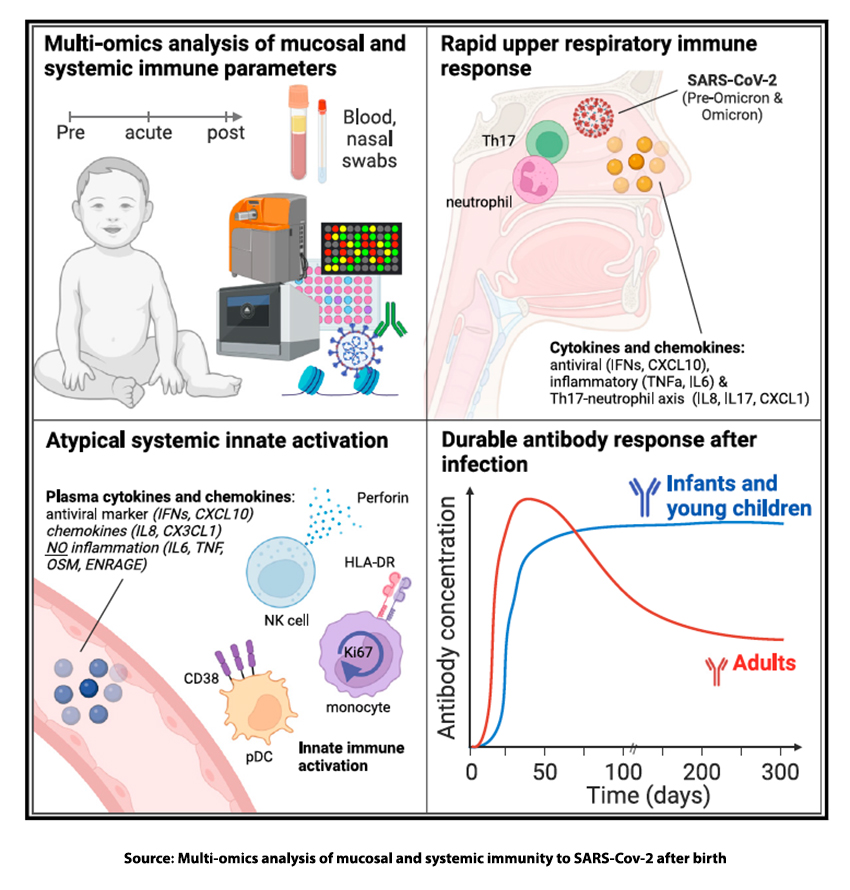
- Activation of the immune response in infants and young children is primarily driven by innate immune responses at mucosal surfaces, particularly in the nose – increasing levels of pro-inflammatory cytokines, including alpha-interferon, which inhibits viral replication. There is increased activation of innate immune cells such as monocytes. one of the first cell types to respond to the virus, and whose activation is associated with the development of symptoms such as fever and cough. [1] In contrast, adults with COVID-19 show elevated levels of inflammation in the blood, suggesting a more systemic immune response.
- Infants and young children mount a robust antibody response, with high levels of anti-Spike IgG and IgA antibodies detected in both serum and nasal swabs. However, this antibody response in infants and young children varies with the COVID variant and maybe most protective against the Omicron variant.
- In adults, antibody levels rose more quickly than in infants but declined just as rapidly – a 10-fold reduction over six months. The blood-borne antibodies remained high for the infants or continued to rise for 300 days.
- Infants and young children have a far more muted induction of those pro-inflammatory cytokines in the blood than adults. It is these chemical mediators that are associated with more severe symptoms of COVID.
“Taken together these findings suggest that the rapid induction of mucosal immunity in the nasal tract might contribute to the mild course of disease in infants and children by containing viral replication in the nose.”
Science supports the idea that in the face of a pandemic like COVID, closing down daycare is not necessarily protective of the children. But those little vectors of disease when kept home will protect the adults caring for them as well as their parents.
[1] You can get a better handle on the effects of these immune cells here.
Source: Multi-omics analysis of mucosal and systemic immunity to SARS-Cov-2 after birth Cell DOI: /10.1016/j.cell.2023.08.044
Special thanks to Bruce Goldman, Senior Science Writer at Stanford Health Care for pointing me to the study.




