"The side effect, the side effects, the side effects." This is what you will hear if you dare to suggest to someone who is walking around with a 300 cholesterol level that maybe should be doing something (real - not some stupid herb) about it. But, on some level I can't blame them? After all, the muscle aches associated with taking statin drugs, e.g., Lipitor are legendary (1). So is Bigfoot. And neither is true.
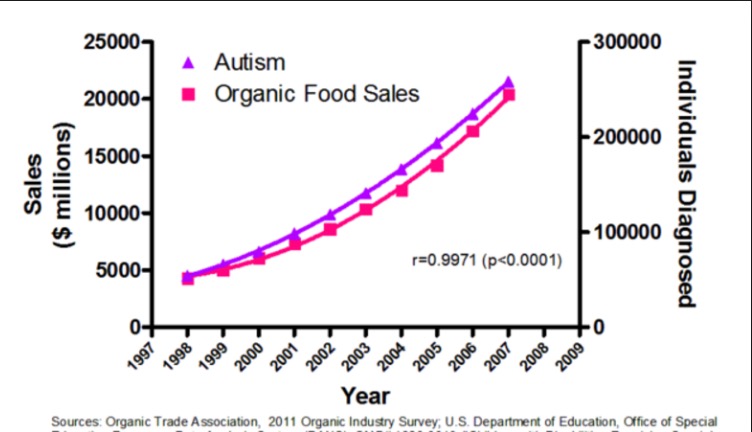
Previous studies of statin connection to muscle pain were observational—studies that tend to yield unreliable data for several reasons. Observational studies involve looking at huge health databases and searching for ... well, pretty much anything that has even a smidgen of statistical significance If you look at enough studies, by sheer chance, you will certainly come up with a close correlation between two events. Something like: People who own goldfish are five-times more likely to prefer Lipton tea to Tetley. If you don't believe me, there is always this. You may have seen it already. There are plenty more out there. Searching huge databases to look for two events that correlate well us called data dredging. It is the bottom of the food chain in the world of studies, and the papers that come out of studies like this are so bad that anyone who knows what to look for will spot the flaws in a few minutes.
It was the findings of observational studies that formed the basis for the connection between statin use and subsequent muscle pain. But it was a big nothing.
A superior method of determining if two effects are related is called a randomized control study, which is designed in advance to measure one or more effects of (anything) on people or animals. These trials start at a particular time and have a endpoint, which will the outcome of the trial— the real effect of a drug or food vs. another population that got a placebo- a control group.
The goal of a very large randomized control study (called ASCOT-LLA) (2), was "to establish the benefits of lowering cholesterol in diabetic patients with well-controlled hypertension and average/below-average cholesterol concentrations, but without established coronary disease." ASCOT-LLA began in 1999 and was stopped in 2002 after it became apparent that cardiovascular events were significantly lower in the drug treated group. (3)
It sure worked, but what about the side effects? This is where it gets interesting. Here are the key findings:
- "[R]eports of muscle-related adverse events [in blinded studies] and erectile dysfunction were similar in both statin and placebo groups. Reports of cognitive dysfunction were extremely rare."
- "By contrast, during the nonblinded, nonrandomized phase, muscle-related symptoms were 41% more common among people taking atorvastatin compared with those who opted not to take the statin..."
The essential finding within the study is what is called the nocebo effect —when patients who get a placebo in the trial nonetheless report symptoms. This effect it obvious here. When the study was blinded—the patient didn't know whether he/she was getting drug or placebo—nothing went wrong. It was only when the patients knew that they were getting a drug that their symptoms showed up. The power of the mind.
And this one is rather interesting:
- Sleep disturbance was noted in 210 per year placebo patients, but only 149 per year in those who got the drug. No—I have no idea what this means. There is no plausible biological mechanism, and it is probably not real
There two principal limitations of the study. First, the results were self-reported, a notorious method of ending up with inaccurate data. But it can be reasonably assumed that self-reporting errors would be similar in both groups. With such a large number of nocebo patients reporting symptoms, inaccurate data is unlikely to be a factor. The other limitation was dose. All participants were given a very low dose of atorvastatin, 10 mg. The recommended dose ranges from 10-80 mg, with 10 mg typically being the starting dose. Depending on the severity of the lipid disorder, 20-40 mg per day is typical.
The criticism of the limitations of the study are valid, but this does not make the results incorrect. No trial is ever perfect, but this one is pretty good, and its ability to demonstrate to demonstrate the nocebo effect for statins is particularly important, since they are widely used and do their job rather well.
Notes:
(1) Lipitor is the brand name for atorvastatin. It was sold by Pfizer and made more money than any other drug in history.
(2) Short for Anglo-Scandinavian Cardiac Outcomes Trial—Lipid Lowering
(3) Once a drug shows a benefit, in this case cardiovascular, it becomes unethical to keep giving participants a placebo.



