Mention osteoporosis-preventing nutrients and most people will think of calcium and vitamin D, even though my colleague Dr. Dinerstein recently wrote they might not be effective in preventing fractures. A recent study in mice, however, suggests a new direction research might take — assessing the impact of dietary fiber.
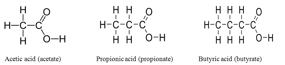
Dr. Mario M. Zaiss from Universitätsklinikum Erlangen, Erlangen, Germany and colleagues pointed out that short chain fatty acids (SCFA), which are the main products of microbial fermentation in the gut, are known to "modulate immune responses of the host." Further, they note that such immune system activation is linked to the status of bone. Thus, they hypothesized that increasing amounts of SCFA might protect bone status.
This hypothesis was tested by three experimental approaches:
- Supplementation of drinking water with SCFA — those with either 2, 3, or 4 carbon chains (1) for periods of 8 weeks. This was done in both normal and ovariectomized (OVX) mice (a model of human post-menopausal bone loss).
- A high fiber diet
- Transfer of specific gut bacteria of types found early in the progression of rheumatoid arthritis.
Water supplementation with SCFA significantly increased the SCFA concentration of treated mice's blood compared to that of untreated animals. CT scans of the tibia of the animals indicated a positive effect of treatment on bone density. Further, the treated mice had a significantly decreased marker for bone resorption (CTX-1) as well as significanly decreased levels of osteoclasts — the cells that break down bone. Importantly, the levels of osteoblasts, cells that form new bone, were normal. When OVX mice were so treated, they didn't experience the bone loss seen in untreated mice.
Next, mice were given diets high in fermentable fiber for 8 weeks, and the effects on bone were compared to those of mice fed a standard diet. Again, the fiber-consuming animals had increased bone mass, decreased osteoclast numbers, and decreased CTX-1 levels compared to the control mice. And again, numbers of osteoblasts were unchanged.
Finally, the investigators transferred bacteria (Prevotella species) to experimental mice. These bacteria are often found in animals suffering from rheumatoid arthritis. These bacteria didn't produce the SCFA that other types did, and they didn't have the beneficial effects seen as a result of the earlier experimental protocols.
Their analyses of their data indicated that SCFA, specifically those with 3 and 4 carbons, significantly suppressed osteoclastogenic signaling entities —TRAF6 and NFATc1, meaning that these SCFAs strongly suppressed differentiation of osteoclasts from precursor cells. At the same time, no consistent effect was seen on osteoblasts. Further investigation indicated that the SCFA stimulation significantly induced glycolysis in the osteoclast precursors. Since transformation to mature osteoclasts depends on oxidative phosphorylation, not glycolysis, this finding indicates a dampening effect on the production of mature osteoclasts.
The authors concluded:
[T]herapeutic supplementation of SCFA or diets increasing the endogenous production of SCFA may provide a powerful instrument to balance osteoclast activity and inhibit bone resorption.
Obviously, this technique is not yet ready for prime time — more experimentation in animals and humans is needed before we can say that the same mechanisms would be seen in humans, or how much fiber might be needed to produce effective levels of osteoclast inhibition in people. However, what it does do is support the concept that dietary fiber can be a valuable part of healthful diet.
1.