It is the 100th anniversary of the 1918 Spanish flu (1,2) pandemic, and the date is not the only similarity between the two. While it is impossible that the morbidity and mortality that is being caused by this year's H3N2 strain (3) will even approach that of the monster that infected 5% of the world, killing 2% of it, 100 years ago, there is one troubling feature that this year's strain shares with its centennial cousin. Flu typically kills because of secondary infections, usually pneumonia. While both "18s" do this, they also kill people directly. This is the scary part.
Fortunately, the fast-killing cases of flu are rare, but it still dominates the news. Children seem to be more susceptible rapid deaths. Cases have been recently reported in Florida, California, and Connecticut. And it may be growing, especially as new strains emerge (4). The cause of fast deaths is very different from that normally seen in flu death. It is more insidious, harder to prevent and little can be done about it. One hundred years ago there were reports of people dying within hours of becoming ill.
"Victims died within hours or days of their symptoms appearing, their skin turning blue and their lungs filling with fluid that caused them to suffocate."
The 1918 Flu Pandemic. Source: The History Channel
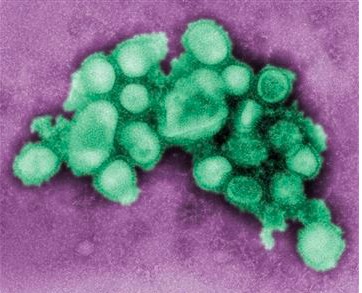
Influenza virus: Image: CDC
What is happening that so radically alters the response of the body to an infectious pathogen? The speed is the clue. If the rapid deaths from flu conjure up thoughts of anaphylaxis (e.g., peanut allergies) it's because they are different versions of the same process - an overload of the immune system because of proteins called cytokines (5). American Council advisor, and infectious disease expert Dr. David Shlaes explains:
Cytokines are small proteins secreted by a number of different cells in the body. They serve to signal other cells for various purposes. In the immune system, this signal can turn on or off various immune and inflammatory responses. They are the "first responders" in the lungs during a flu infection, where they can send out signals that attract more cytokines. Once the normal balance between immune and inflammatory responses is abrogated and inflammatory cytokines are produced in high concentrations a cytokine storm can result.
This leads to the dilatation of small vessels and leak of body fluids through capillaries causing fluid accumulation in the soft tissues (edema) and in the lungs. This in turn leads to a decreased blood pressure The release of these cytokines also causes fever. The entire picture resembles what occurs in sepsis. The result of all this is often fatal.
Dr. David Shlaes, Infectious disease expert and American Council advisor.
Eventually, this very bad flu season will end. When the numbers are tallied up this may end up being the worst flu season in a generation. Since flu is extremely contagious there isn't much you can do except get vaccinated. Even though this year's vaccine covers only about one-third of circulating strains, it is helpful even if you contract a strain that is not in the vaccine because the vaccine gives partial immunity (6).
There is very little good news this flu season, except that the bad news has been exaggerated. Deaths from cytokine storm make good headlines but they are rare. Far more people will die from complications of flu rather than the virus itself. All you can do is roll up your sleeve. Refusing the vaccine, as imperfect as it is, in a year like this is like playing "Spanish Roulette." This is not the year to play. Too many bullets in the chamber.
NOTES:
(1) There was very little "Spanish" about the Spanish flu. Its name was a result of World War I geopolitics. Spain was neutral in WWI and its press was free to report the details of the flu. Other countries had their news censored and details of the flu were suppressed to maintain morale among troops. Also, Spanish King Alfonso XIII came down with a nasty case, which only served to further spread the misnomer. No one knows where it really started.
(2) For a fascinating look at the epidemiology of the 1918 flu see Ruth Craig's article in The Conversation.
(3) My colleague Dr. Julianna LeMieux predicted that H3N2 was going to be trouble in early January.
(4) It is thought that exposure to new flu strains provokes a stronger immune response in people who have not been exposed to a similar strain. This is one reason for the increase in rapid flu deaths.
(5) For a (much) more detailed overview of cytokines, see a ScienceDirect summary of a book chapter about asthma.
(6) Dr. Richard Whitley, Distinguished Professor of Pediatrics, Division Director Pediatric Infectious Diseases at the University of Alabama, private communication.


