Prostate cancer, now considered the most common cancer in men, especially African-Americans, was uncommon until the 1950s. Earlier, a blood test identifying prostate-specific antigen, PSA, was developed for use in “rape kits” to provide criminal evidence. It was never designed as a screening tool for prostate cancer that it has become. Today, national guidelines recommend screening with PSA for men age 55 to 69, a recommendation that only 40% of men follow. But what happens after a PSA test is termed positive?
BIOPSY
A biopsy, removal of a small bit of tissue and examination for cancer cells, remains the gold standard in diagnosing prostate cancer. These biopsies are now performed in an office setting, using topical anesthesia. It involves using a needle to obtain tissue from the prostate through the rectum. Twenty years ago, the routine biopsy protocol called for six needle cores. Because it was performed without imaging, it missed many cancers deep within the prostate. The number of tissue samples taken was expanded to 12 and up to 96 cores. Needle biopsies are generally safe but, like all procedures, can cause serious complications. An infection that can require prolonged antibiotic therapy is the most common. Nowadays, biopsies are guided, meaning that imaging through ultrasound or MRI, are used to direct the needles to areas of concern.
DOPPLER ULTRASOUND
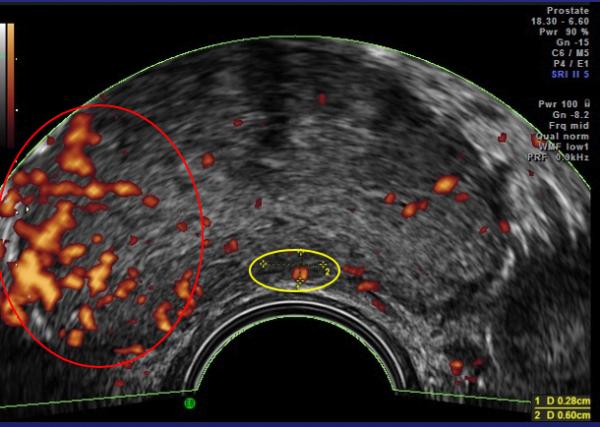
In 1994 Prof. Francois Cornud in Paris developed a better way to sample the tissue of the prostate using Doppler ultrasound. Sound waves are reflected by different tissues at different speeds, creating an image. These doppler images show tumor vascular flow the same way the Weather Doppler shows tornadoes. The presence of tumor-related blood vessels poses a hazard during the biopsy, where they can be inadvertently “nicked,” resulting in bleeding, and their presence indicates a more serious, “aggressive,” tumor. Effective cancer therapies shrink these arteries, making this 10-minute examination both safer and a means of indirectly monitoring treatment.
Since prostate cancer is, in many instances, slow-growing, early cases are often managed by watchful waiting, without invasive surgery or chemotherapy. Ultrasound imaging that detects increased tumor vascularity allows patients with biopsy-proven cancers to come in for regular scans to see if their disease is stable or if more aggressive treatment is indicated.
Computers have greatly enhanced medical imaging. Current ultrasound systems capture 250 images in 10 seconds in all directions. These “multiplanar” images are reconstructed by the computer allowing us to see the prostate capsule far more clearly than an MRI. This is important as the extension of cancer outside the capsule to the surrounding tissue implies possible tumor spread to other organs.
These technologies can focus the doppler’s sound waves on specific areas and additional data describing blood flow obtained. This data can be combined to generate a quantitative reading of the tumor vessel density to serve as a treatment guide. Vessel density of 15% is found in aggressive cancers requiring intervention, while densities of 1-2% are noted in most low-grade tumors, that can simply be monitored.
MRI IMAGING
MRI has been the “gold standard” and greatly improved with the addition of contrast “dye,” which has occasional serious allergic reactions. The presence of inflammation, both acute and chronic, makes MRI reading confusing since the vessels of infection are similar to those feeding cancers and have resulted in false positives and unnecessary biopsies. MRI scans are often used to guide the biopsy needle. Recent advances in the clinical data from ultrasound are so accurate that it is replacing MRI and follow up biopsies in many patients. New ultrahigh-resolution ultrasound units and computerized optical devices are now used instead of MRI for diagnosing PC in Europe and guiding biopsies without x-rays.
OUR EXPERIENCE
Located in mid-town Manhattan, we have cared for many of 911’s first responders who have, unfortunately, developed cancer at an extraordinarily high rate. Fortunately, most of these are low-grade tumors, and many of New York’s heroes prefer yearly monitoring with sonograms and agree to be biopsied when a significant change is noted in comparison. Our center’s results on over 50,000 scans, since 1974, have shown low-grade cancer pose a risk to life in less than 1% of these patients over a 10-year time frame. As radiologists, it took time for us to appreciate that cancer tissues identified under a microscope have different clinical paths and that, for some, the malignancy acts more like a chronic disease than a life-threatening illness.
TREATMENT
In addition to watchful waiting, treatment options include surgical treatment and radiotherapy. Radiation treatment may use “radioactive seeds” implanted in the local tissue or delivered by various external beam devices and are useful when the prostate tumor has expanded outside the gland. Hormone and 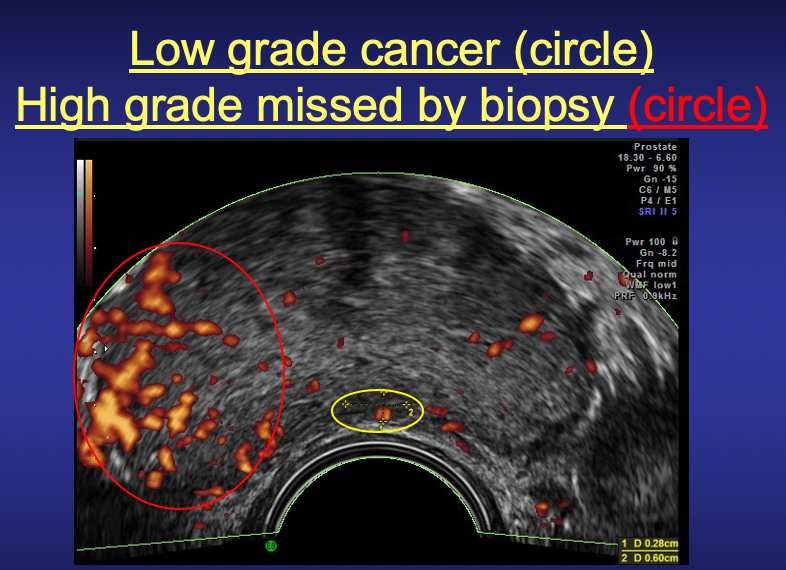
chemotherapy are conventional alternatives. It is advisable to seek medical opinions on personalized healing options as side effects occur and treatment is best individually tailored. Recurrence may occur following successful initial therapy with any treatment modality, and Doppler ultrasound with MRI is useful in detecting any regrowth as this image shows.
Sources: Bard R: Contrast MRI and 3D Doppler Ultrasound presented at the 109th Annual Meeting of the American Roentgen Ray Society 2009
Bard R: Contrast MRI Atlas of Prostate Cancer
Bard R: Editor; Image Guided Prostate Cancer Treatment



