
Pain patients should be celebrating (at least a little) because an abstract from the 2020 meeting of the International Anesthesia Research Society asks some very interesting questions, the details of which were just published in an article in Pain Medicine News. The title itself is intriguing: "Post-op Opioid Prescribing Often Ignores CYP2D6 Pharmacogenetics," the keyword being "ignores." Just as many pain patients have been ignored, the same has largely been true of the science: Why do some people get adequate pain relief from a certain dose of an opioid while others do not? More on this below.
Back in 2018, I wrote an article called "Opioid Policies Based On Morphine Milligram Equivalents Are Automatically Flawed" in which I argued that the simplistic assumptions used to establish maximum daily doses (1) of opioids were so flawed that the same dose of a given drug could be too low for one person and too high for another.
Although body weight can be a determinant of dose, it is possible that a 90-pound woman might require a higher dose for pain control than a 200-pound man. The reason – significant genetic differences in the liver enzymes (called CYPs) (2), which are responsible for the metabolism of numerous drugs and other chemical substances. The amount and composition of the CYPs vary from one person to another because of genetic factors.
To further complicate matters, CYP metabolism can either decrease or increase the blood levels of the active opioid, depending on the drug in question. Some opioids have no analgesic properties until they are metabolized (activated) to form the active drug, while others are active on their own but are broken down to form inactive fragments by other enzymes (3).
1. Activation
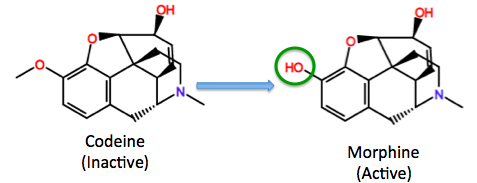
Metabolic activation of codeine by CYP2D6 to form morphine, the actual drug. People who have abnormally low levels of CYP2D6 will probably not find codeine useful. The green circle shows the site of metabolic activation. The hydroxyl group is required for binding to opioid receptors.
2. Deactivation
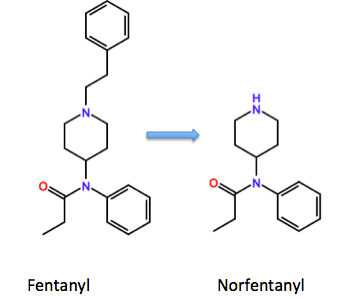
Metabolic inactivation of fentanyl by CYP3A4 to form norfentanyl (inactive). People who have low amounts of functioning CYP3A4, either because of genetics or the presence of another drug that inhibits the enzyme, are more likely to overdose because the fentanyl isn't cleared from the body at a "normal" rate.
Now for the good news
The meeting presentation by Daniel B. Larach, M.D., an assistant professor of clinical anesthesiology at the Keck School of Medicine of USC in Los Angeles, asks whether some patients, because of their genetic makeup, will suffer inadequate post-surgical pain control. The answer is yes – something that chronic pain patients have been maintaining for years. This can happen when the function of CYP2D6 is impaired.
In a new study, Larch reported that 20,885 people underwent CYP2D6 genotype testing (4). Of these, 8,157 had never taken an opioid before (opioid-naive) but received a prescription for one following surgery. A total of 628 of the 8,157 (7.7%) were defined as poor or intermediate metabolizers. Let's look at the 628.
The analysis found that 361 of the 628 poor and intermediate metabolizers who received opioid prescriptions (57.5%) were prescribed either tramadol, codeine, or (most often by a wide margin) hydrocodone (5). Larach's conclusion will be sweet music to the ears of pain patients (emphasis mine):
“That’s a significant portion of patients who may not respond to the medication that they’re getting...And that can be important for a variety of reasons—the most important being they’re less likely to get adequate analgesia, which puts them at risk for chronic postoperative pain."
And the next quote will most certainly resonate with the millions of pain patients who have perennially been treated like addicts:
“There’s [the] risk [of a patient being] labeled as a potential abuser if you require more refills and prolonged opioid consumption."
D. Larch, M.D. (both quotes)
Larisa H. Cavallari, PharmD, BCPS, an associate professor of pharmacotherapy and translational research at the University of Florida Gainesville, was not surprised. Her group also studies (6) postoperative pain. Using genetic information as a guide resulted in "significantly lower opioid use without compromising pain control."
“It makes sense to genotype beforehand, especially if it’s an elective procedure and there’s plenty of time to do that...Then the results can be back in time to inform the prescriptions for postoperative pain management.”
Larisa H. Cavallari, PharmD
What should be obvious by now is that if a simple genetic test can guide the selection of post-op opioids it could also be used to help determine the needs of chronic pain patients. Science could be used to determine the correct dose of the correct drug for an individual rather than the arbitrary one-size-fits-none system under which we now operate.
What a difference one test could make in the lives of millions.
NOTES:
(1) Nonetheless, the "suggested" maximum doses, which were BS, to begin with, became laws. We all know what happened then.
(2) CYP is short for Cytochrome P450, a hugely important family of enzymes responsible for most metabolism in the body. The P450 stands pigment-450 nanometers, the maximum UV absorbance of the enzyme when bonded to carbon monoxide.
(3) It's even worse than what I showed. Drugs can have multiple sites of metabolism, and the metabolites themselves can also undergo secondary metabolism. It is not unusual to identify 10 different metabolites of a single drug in blood or urine.
(4) "The CYP2D6 genetic test is used to predict how you will respond to a large number of different medications." Source: Mayo Clinic.
(5) Nearly all of these individuals received hydrocodone, which the authors said has a “controversial” pharmacogenetic relationship with cytochrome P450 2D6 (CYP2D6). In other words, the pharmacokinetics of hydrocodone is not well understood.
(6) See Clin Pharmacol Ther 2020;107[suppl 1]:S20)



