Do we maximize to save lives or save the economy -- health or wealth?
While closely related, these goals require us to prioritize very different populations. To save the economy, we need to vaccinate the most mobile economy quickly, the 18-65 year-olds, get them safely working and socially engaged. During the interim, those most at risk would continue to isolate. You can find the underlying model discussed here and some of the ethical concerns discussed here.
But the ACIP was rightly concerned with overwhelming the healthcare system and initiating a series of life and death triage decisions over whose lives to save. They chose to maximize saving lives, writing:
"These benefits include the reduction of SARS-CoV-2 infections and COVID-19–associated morbidity and mortality, which in turn reduces the burden on strained health care capacity and facilities; preservation of services essential to the COVID-19 response; and maintenance of overall societal functioning."
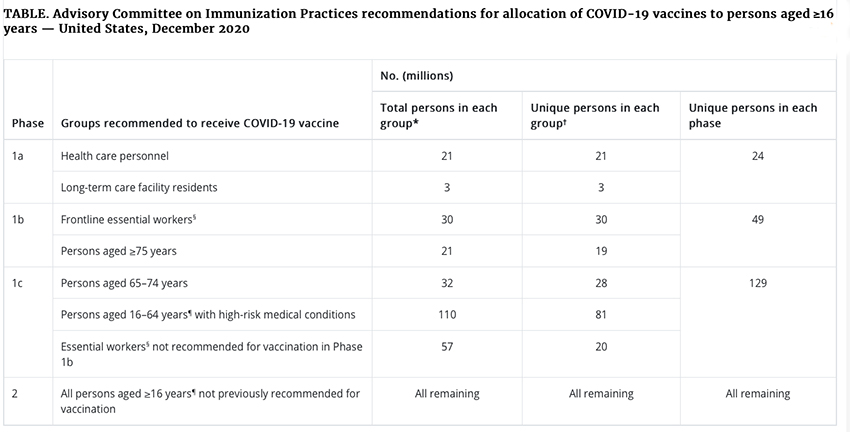 Here is the table from the ACIP latest update, and you can see how the population being treated doubles, then expands six fold in the next phases of vaccination. The final push involves roughly half of our population.
Here is the table from the ACIP latest update, and you can see how the population being treated doubles, then expands six fold in the next phases of vaccination. The final push involves roughly half of our population.
Ethical Considerations
The decisions surrounding vaccine allocation have taken into account four pillars of ethical considerations [1], but remember, ethical questions by their very definition frequently have no one true answer.
Maximize benefits and minimize harms
"to both individual recipients and the population overall…. based on scientific evidence…"
While we can broadly identify at-risk populations, it becomes more challenging to stratify within groups. For example, there is an extensive range of risk among healthcare workers. Those we might suspect of most significant risk, nurses working in ICUs, are at much lower risk than nurses and their support staff working on medical and surgical floors. And do we, let alone can we, further identify the ethnicity, gender, and co-morbidities that heighten the risk within these subgroups? The same may hold if we look at "essential" workgroups. Public transportation workers are both more essential and at higher risk in New York City than in Los Angeles. Urban farmers may not be as critical as those in the heartland.
Promote justice
"intentionally ensuring that all persons have equal opportunity to be vaccinated, both within the groups recommended for initial vaccination, and as vaccine becomes more widely available."
"removing unfair, unjust, and avoidable barriers to vaccination that disproportionately affect groups that have been economically or socially marginalized."
The words unfair and unjust come with a justifiable halo of good, but what do they really mean? The "vaccine hesitancy" among African Americans, a group at increased risk, has long-standing medical roots. It will not go away with more "education," and the impact of influencer endorsement, be it a celebrity or religious leader, is unclear. More concretely, what hours are vaccines available? Many of the economically disadvantaged hold jobs where you don't get time off; a 9 to 5 vaccination clinic doesn't meet a 7 to 6 laborer's needs.
Mitigate health inequities
"Health equity is achieved when every person has the opportunity to attain his or her full health potential, and no one is disadvantaged from achieving this potential because of social position or other socially determined circumstances."
"Vaccine allocation strategies should aim to both reduce existing disparities and to not create new disparities. Efforts should be made to identify and remove obstacles and barriers to receiving COVID-19 vaccine…"
We need to look no further than Stanford for the difficulty of this principle. To avoid disparity Stanford's hospital developed an algorithm using ethicists and guidelines. Of the 5000 initial doses, five were given to medical residents caring for patients, later corrected to 7. Besides again demonstrating the artificial in artificial intelligence, especially concerning medicine, the incident shows that unintended consequences can follow despite good intentions. The intent to achieve health equity is not a guarantee of an outcome.
Promote transparency
"The underlying principles, decision-making processes, and plans for COVID-19 vaccine allocation must be evidence-based, clear, understandable, and publicly available."
"… Transparency includes being clear about the level of certainty in the available evidence and communicating new information that might change recommendations in a timely fashion."
The state and local governments are failing in this regard, as have I, along with scientists, public health officials, and journalists. It is tough to explain complex science and to have a nuanced discussion when all you are offered is 150 characters or a minute of video. And to be fair, there may be a fair amount of scrambling of the receivers' message, influenced by feeling over thinking, and comfortable over hard. Changing evidence is described as "gotchas," not the process of science.
The ACIP has made a concerted effort to provide guidelines to the States for allocating vaccines. As with all policies, it involves tradeoffs. They have been more transparent than many on which tradeoffs they have made. We can disagree; the nature of ethics inevitably requires uncertainty. But we are wasting a good deal of our national energy in wringing our hands about our position in line; energy better spent on speeding up the process, not endlessly debating it.
[1] The Advisory Committee on Immunization Practices' Ethical Principles for Allocating Initial Supplies of COVID-19 Vaccine — United States, 2020




