Health care personnel (HCP) are defined as
“…all paid and unpaid persons serving in health care settings who have the potential for direct or indirect exposure to patients or infectious materials, including body substances (e.g., blood, tissue, and specific body fluids); contaminated medical supplies, devices, and equipment; contaminated environmental surfaces; or contaminated air.”
That is a lot of individuals and includes many without direct patient contact; you only need to be working in that potentially contaminated environment. Let’s start with a few limitations in our data collection, a key finding in a report by the National Academies of Sciences, Engineering, and Medicine (NASEM).
- It is difficult to identify the source of exposure, community or occupational (at or related to work)
- Reporting health care as an occupation was only required beginning in May. Despite the requirement, occupation is frequently not reported, and reporting varies among states. Infection with COVID-19 is most likely under-reported.
- The absence of a uniform national dataset makes comparison, analysis, conclusions, as well as subsequent recommendations “impaired.”
- The psychologic burden is similarly uncertain
- Simply put, our data collection is just this side of garbage in, garbage out. [1]
Given these limitations, apply as much uncertainty as you wish to the following information. The CDC issues any number of weekly morbidity and mortality reports on health care personnel. I made use of two; see sources for the citation and links.
- Most HCP with COVID-19 were female (79%)
- 16–44 years old (57%) median age 41
- Not hospitalized (92%)
- Lacked all ten underlying medical conditions (56%) [2]
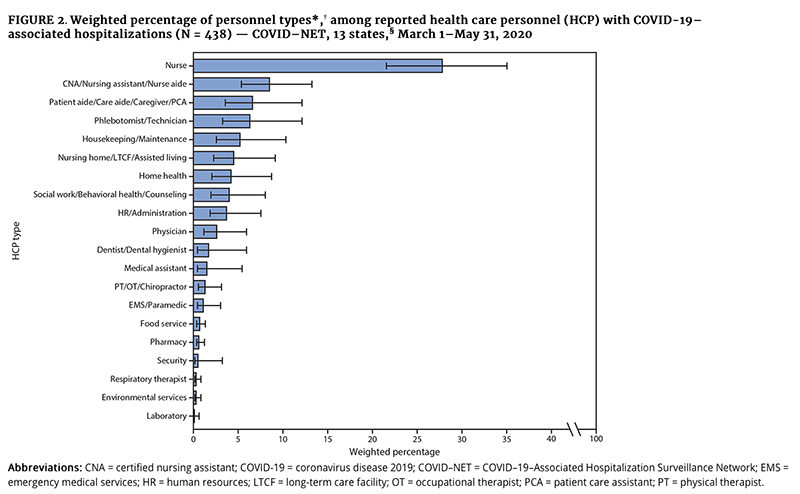
- Nurses were the most frequently identified single occupation type (30%)
- Nursing and residential care facilities were the most common job setting (67%).
- Of the 8% hospitalized, 25% were admitted to the Intensive Care Unit
- 641 deaths -a higher percentage of fatal cases occurred in males, aged > 65, Asians, Blacks, and persons “with any of the 10 underlying medical conditions.” 92% of deaths involved HCPs with an underlying medical condition. With a total of 100,000 cases involving HCP, the case fatality rate is 0.006% - for comparison, the case fatality rate in the US is 1.9%
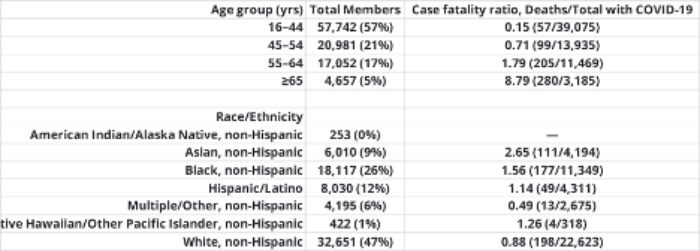
This incomplete table is enlightening.

The individuals at the most significant risk are the nurses and the aides with prolonged direct contact. The administrative staff includes a group of unit clerks that work directly on the wards. The bulk of cases are outside acute care facilities, e.g., hospitals and ambulatory care centers. And it is these sites that have documented problems with “inadequate staffing and PPE, and training in infection prevention and control.”
The second MMWR looked explicitly at the 6,760 adults hospitalized between March 1st and May 31st whose occupation was known to be an HCP. At this time, HCP accounted for 5.9% of admissions, similar to the 8% in the prior report. A similar percentage had severe disease requiring intensive care (27.5%), and 4.2% subsequently died for a case fatality rate of 3.6%, significantly different from prior surveillance. The most common co-morbidity in this study was obesity (72%), while in the prior study, it was cardiovascular disease (18%). The real value here is the delineation of the roles of the infected HCPs; 66% were involved in direct patient care, as this graphic depicts.
Finally, we can note a new dataset from anesthesiologists; a group felt to be at high-risk because they are involved in placing breathing tubes in patients (intubation) being placed on mechanical ventilators and because they often are “in-charge” of intensive care units. The study out of the UK suffered from the same data issues as the CDC reports. It found a 5.8% of COVID-19 deaths were among HCPs. They found that direct care increased the risk of developing a COVID-19 infection 2 to 4 fold. But here is their most interesting finding. Despite being in the ICU, those working in the ICU had half the risk of PCR-positive infections as those HCPs working on medical wards. Working in the ICU was protective as compared to those working in “front-door” roles. Why would that be?
Two-words. Universal precautions - the medical version of masks and social distancing.
Consider hospitals. They have the most symptomatic of patients, the ones we believe are at the peak of shedding viable virus to transmit to others, and the most significant direct contact. But hospitals have a buffer between their inside and the outside world; their airlock is the Emergency Department. In the ED, the cases of COVID-19 are identified and sent to specific wards and rooms – all the identifiable COVID-19 transmitters are isolated, an extreme form of social distancing. From that point forward, they are treated by staff wearing masks and gloves, and the patients, when moved about, are covered with masks. The ICUs apparently have a lower transmission risk because those patients are often on ventilators, and the airborne components of COVID-19 remain in ventilator circuits, not in the room air. And once again, the people in direct contact with them are masked, gloved, and, if necessary, gowned. In hospitals, universal precautions and respiratory isolation are not options; they are the mandates of reasonable care. And if you look at the infection rates of hospital HCP, universal precautions work.
The higher rates of HCP infections are in assisted living, nursing homes, etc. Now part of this may well be the patients themselves. Given their age and debilities, they are the kindling in the COVID-19 fire. But there is no ED “airlock” in these facilities. They have stopped the influx of family by prohibiting visitation, but not the flow of staff that work at more than one site, who can track COVID-19 from one facility to another. Critically, they do not employ universal precautions; everyone is not necessarily quarantined. The staff is inadequately trained in these techniques, and evidently, the PPE to utilize in these procedures is lacking. Could this explain the four-fold greater incidence of HCP infections?
I am trying to make two points. First, as incomplete and unclear as it is, the data strongly suggests that HCPs, while being very exposed to COVID-19, manage to avoid being susceptible. Part of the reason is their ages and co-morbidities. But to my second point, an important additional component is how they behave, their wear masks and social distance, end of the discussion. The data is there in the infection rates of HCPs, hidden in plain sight.
[1] For those who have significant concerns about the posterchild of data collection, electronic medical records, none of this is surprising. NASEM points out that our data collection has “substantial variation ... in data collection, recording, and reporting practices, … insufficient prioritization of current systems to ensure more accurate and consistent data… poor functionality and interoperability… and a need for better training on data collection…”
[2] “diabetes mellitus; cardiovascular disease (includes hypertension); severe obesity (body mass index ≥40 kg/m2); chronic renal disease; chronic liver disease; chronic lung disease; immunosuppressive condition; autoimmune condition; neurologic condition (including neurodevelopmental, intellectual, physical, visual, or health impairment); and psychologic/psychiatric condition.”
Occupational COVID-19 risk for anaesthesia and intensive care staff – low-risk specialties in a high-risk setting Anesthesia DOI: 10.1111/anae.15358




