Why microbes kill some people, but not others is probably the hardest question in all of medical microbiology.
For many deaths, the answer is obvious. Old age or underlying health conditions can make a person more vulnerable to infectious disease. But these aren't the only reasons. Sometimes, otherwise healthy people acquire flesh-eating bacteria, or others fall victim to a brain-eating amoeba. What makes these deaths so odd is the indisputable fact that millions of other people come into contact with the same microbes, but nothing happens to them. Why?
Something similar is happening with COVID-19. For most people, the virus causes mild symptoms or none at all. For some, usually the elderly or infirm, the virus is severe or even deadly. But once again, the virus only kills a small fraction of the people it infects. Why?
One answer scientists discovered involves the cytokine storm. Cytokines are messenger molecules that allow immune cells to communicate. A cytokine storm occurs when too many pro-inflammatory cytokines are released, resulting in respiratory distress, multiple organ failure, and death. Like the above examples, why some people develop cytokine storms and others don't is unknown, but the answer likely involves an individual's genes, perhaps those that encode a set of proteins known as the Major Histocompatibility Complex (MHC).
 Some Antibodies to COVID Attack the Body
Some Antibodies to COVID Attack the Body
Now, a team of researchers at New York University (NYU) report that deadly cases of COVID are linked to autoantibodies, i.e., antibodies that attack the body. In other words, COVID appears to trigger an autoimmune response in some people.
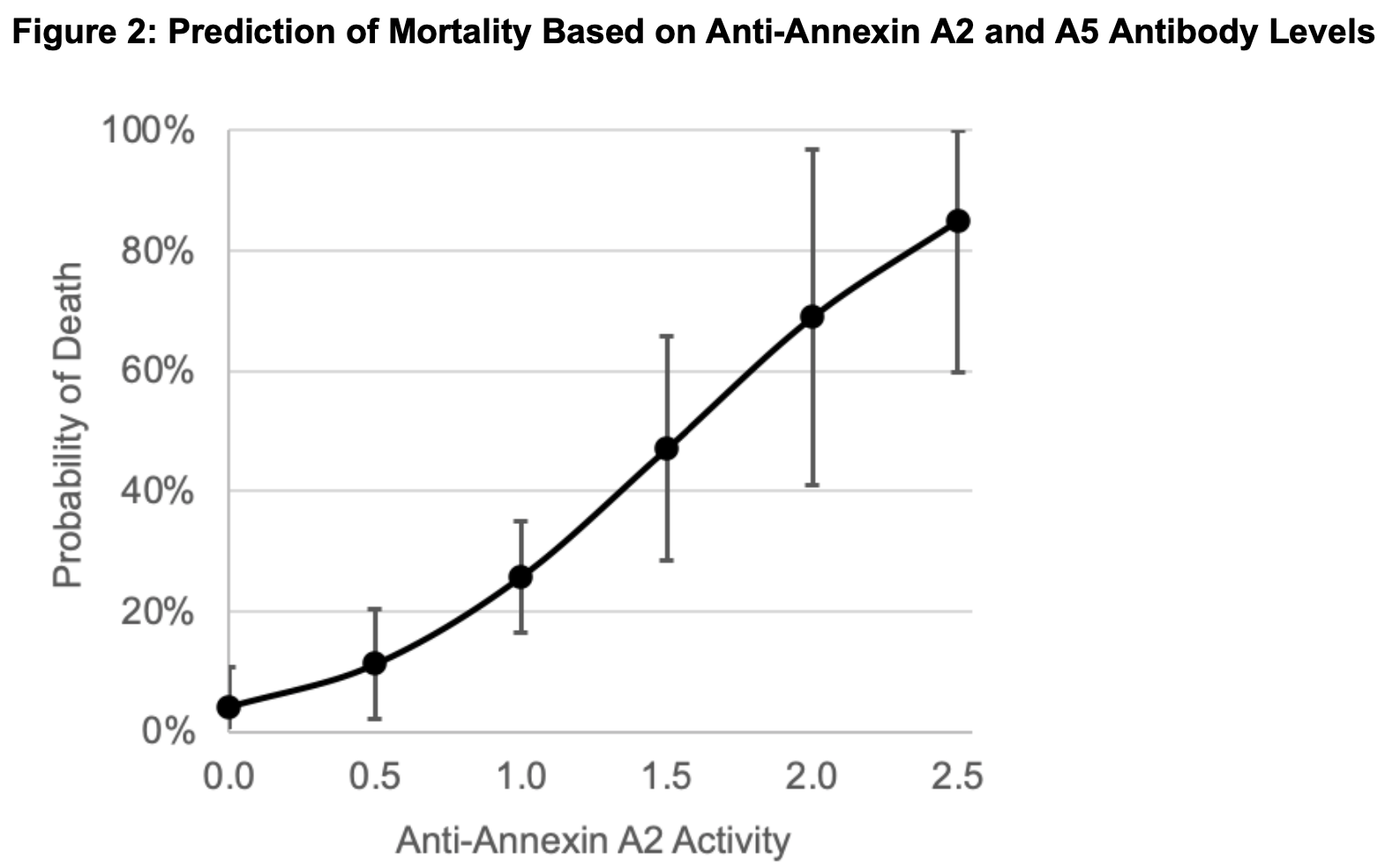
Specifically, the authors examined the levels of antibodies against Annexin A2, a protein found in the lungs that plays an important role in anti-inflammatory processes and maintaining the structure of blood vessels. Antibodies that target it, therefore, may exacerbate respiratory problems caused by COVID.
The researchers analyzed the antibody levels in 86 patients who were hospitalized with COVID. Of these patients, 28 were not critically ill, 36 were critically ill, and 22 died. Using logistic regression, the authors were then able to determine an association between antibody level and death. Indeed, using margins analysis, the team showed that the probability of death increased as a patient's anti-Annexin A2 antibody levels increased.
Limitations
There are several limitations, a couple of which are worth noting. The paper is on the medRxiv preprint server and is not yet peer-reviewed. Also, a single association study is insufficient to conclude causation, so it's not yet possible to say definitively that anti-Annexin A2 antibodies were responsible for the higher probability of death. But it's tempting to speculate that they played a role, especially since it is well known that several microbes trigger autoimmune disease. At the very least, anti-Annexin A2 antibody levels seem to predict death, so monitoring them may give clinicians insight into the severity of COVID in a patient.
Source: Marisol Zuniga, et al. "Autoimmunity to the Lung Protective Phospholipid-Binding Protein Annexin A2 Predicts Mortality Among Hospitalized COVID-19 Patients." medRxiv. Posted on 4-Jan-21. DOI: 10.1101/2020.12.28.20248807