Inexperienced journalists commonly make a mistake known as “burying the lede,” or hiding the most crucial aspects of a story underneath lots of distracting and less significant information. Scientists often make an analogous mistake, by emphasizing less important results from their research while minimizing others that are more relevant, especially because they're related to public health.
Case in point: a study published last week in the American Heart Association's (AHA) journal Circulation reported an association between dual use of e-cigarettes and combustible tobacco and increased cardiovascular disease (CVD) risk over a six-year period. The paper's results, as we'll see, clearly support vaping as a low-risk alternative to smoking, but the AHA did its best to downplay this result.
The study
The researchers surveyed 24,027 participants from the Population Assessment of Tobacco and Health (PATH) study, who self-reported their smoking, vaping, or dual-use habits annually between 2013 and 2019. Anyone who had smoked more than 100 cigarettes in their lifetime and reported current smoking was classified as a smoker. If someone reported any current e-cigarette use, they were categorized as a vaper. Participants were classified by “non-use (no current e-cigarette use or smoking), exclusive e-cigarette use, exclusive smoking, or dual use.” These classifications were updated annually.
The researchers defined incident CVD as any self-reported diagnosis of myocardial infarction (MI) or bypass surgery, heart failure (HF), other heart condition, or stroke starting at wave 2 and continuing through wave 5; they also measured MI, HF, and stroke separately.
What they should have led with
Setting aside the broad exposure definitions utilized in this study, which I've criticized previously, the results painted vaping in a rather favorable light:
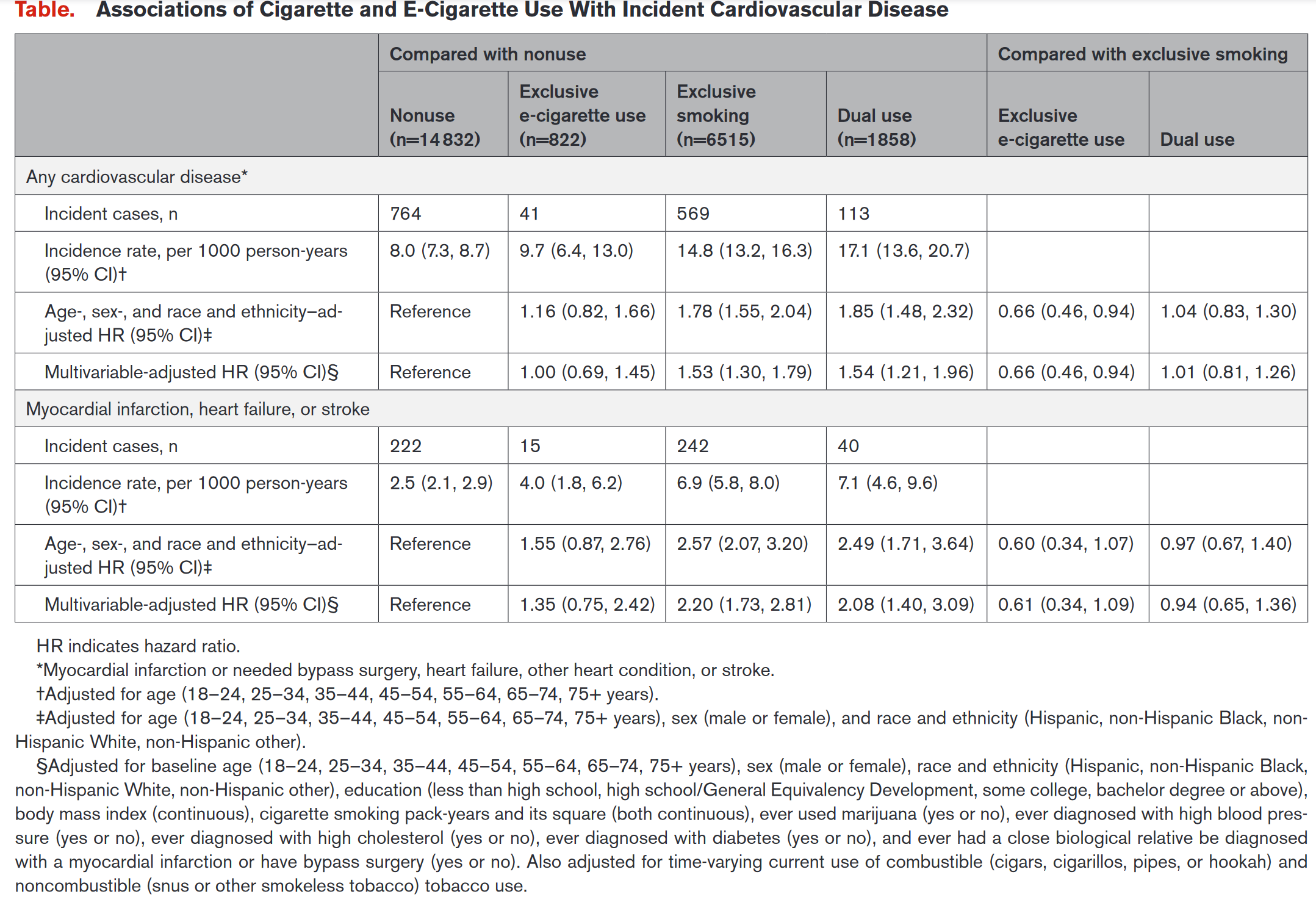
“After adjusting for covariates, participants exclusively using e-cigarettes had risk of developing any CVD condition that did not differ from non-users and higher, albeit non-significant, risk of the MI, HF, or stroke outcome … Compared with smoking, e-cigarette use was associated with 30% to 40% lower CVD risk, although this association was only significant for the any CVD outcome.”
Smokers self-reported 569 CVD events compared to just 41 in e-cigarette users (see Table below). Limiting the results to heart attack, heart failure, or stroke, smokers experienced 242 events, but vapers reported only 15 of these same events. That's a tremendous risk reduction, so the obvious conclusion to draw from these results is that vaping is associated with far less CVD than smoking.
Depending on the specific condition under observation, it appears that vaping poses very little risk whatsoever. But it gets better. The authors went on to note that
“We did not find a significant difference in the cardiovascular risk of exclusive e-cigarette use compared with non-use of cigarettes and e-cigarettes, although analyses were limited by a small number of CVD events in e-cigarette users.”
Read that sentence again. They couldn't determine if the cardiovascular risk of vaping was statistically significant because e-cigarette users experienced too few CVD events. In other words, there was no meaningful association between vaping and increased cardiovascular disease risk. That's the take-home message of this paper. Yet, this is the headline the American Heart Association put on its press release for the study: "No health benefits among adults who used both e-cigarettes and traditional cigarettes."
Even here, though, the results weren't clear. It's possible that the elevated CVD risk of dual-users was attributable entirely to their cigarette consumption. For instance, if someone smoked two fewer cigarettes daily out of a pack of 20, they still smoked 18 cigarettes every day for six years. We don't know if that's what actually happened; the exposure data is too vague to draw such a specific conclusion. But the fact remains: the AHA highlighted the only result that portrays vaping as harmful.
Inconvenient results
I suspect the AHA knows how bad these results look for the campaign against e-cigarettes, because the press release included this very revealing quote:
“While the PATH study is providing essential longitudinal data on the use of traditional and e-cigarettes, as well as on outcomes such as cardiovascular events, the data are self-reported, the study duration is short and the event rate is still low – especially in younger people.
Since e-cigarette use is still relatively new, there is not yet a strong body of long-term evidence to determine the eventual risk of using these products over time … It’s important to remember that even with traditional cigarettes, decades of use and surveillance were needed to provide the strength of evidence we now have confirming the highly significant harm of combustible cigarettes.”
— Rose Marie Robertson, M.D., FAHA, deputy chief science and medical officer of the American Heart Association
These comments prompt several questions. Almost every epidemiological study has some important flaws or limitations. You usually have to read the paper very carefully to uncover those deficits, but the AHA is offering them up in the press release—the document that gullible journalists use to write their stories. Why did the AHA so eagerly highlight PATH's self-reported data, low event rate, and short duration? Moreover, if the PATH results are so incomplete, why did these researchers use them in the first place?
Finally, why did Dr. Robertson imply that future studies may uncover serious vaping-related health risks as earlier research did for tobacco use? We already know that vaping is much less harmful than smoking, so her analogy is unjustified. The long-term risks of any new product are, by definition, unknown. Yet, we shouldn't speculate about what those risks could be, especially when the existing data suggest that the product isn't very harmful.
By way of comparison, no respectable scientist would warn that “Since COVID vaccination is still relatively new, there is not yet a strong body of long-term evidence to determine the eventual risk of receiving these immunizations over time.” People who speculate in this manner are quickly labeled anti-vaccine quacks. But tobacco-control researchers make the same illogical leap when trying to tap dance around the evidence on e-cigarettes. They need to stop.
A growing body of research, arguably including the present study, shows that vaping is a safer alternative to smoking. [1] Until the data show otherwise, let's stick with that conclusion.
[1] Since the new study's results were based on self-reported data and imprecise exposures—how much vaping does “any e-cigarette use” constitute?—I'm inclined to disregard this paper altogether. But if the AHA will use its data to attack dual-use, the organization needs to embrace the favorable results related to exclusive vaping from the same study.




